Shop for Plans
Shop for your own coverage
Plans through your employer
Learn about the medical, dental, pharmacy, behavioral, and voluntary benefits your employer may offer.
Learn
Looking for Medicare coverage?
Adjustment to Cancer: Anxiety and Distress (PDQ®): Supportive care - Health Professional Information [NCI]
Overview
Studies examining the prevalence of mental disorders in cancer patients [
Psychosocial distress exists on a continuum (see the figure below) ranging from normal adjustment issues through the adjustment disorders of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5);[
- Normal adjustment issues.
- Psychosocial distress.
- Adjustment disorders.
- Cancer-related anxiety.
For more information, see Depression and Cancer-Related Post-Traumatic Stress.
Anxiety is often manifested at various times during cancer screening, diagnosis, treatment, and recurrence. It can sometimes affect a person's behavior regarding his or her health, contributing to a delay in or neglect of measures that might prevent cancer.[
For patients undergoing cancer treatment, anxiety can also heighten the expectancy of pain,[
In this summary, unless otherwise stated, evidence and practice issues as they relate to adults are discussed. The evidence and application to practice related to children may differ significantly from information related to adults. When specific information about the care of children is available, it is summarized under its own heading.
References:
- Derogatis LR, Morrow GR, Fetting J, et al.: The prevalence of psychiatric disorders among cancer patients. JAMA 249 (6): 751-7, 1983.
- Massie MJ, Holland JC: Overview of normal reactions and prevalence of psychiatric disorders. In: Holland JC, Rowland JH, eds.: Handbook of Psychooncology: Psychological Care of the Patient With Cancer. Oxford University Press, 1989, pp 273-82.
- Bisson JI, Chubb HL, Bennett S, et al.: The prevalence and predictors of psychological distress in patients with early localized prostate cancer. BJU Int 90 (1): 56-61, 2002.
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association, 2013.
- National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology: Distress Management. Version 2.2023. Plymouth Meeting, Pa: National Comprehensive Cancer Network, 2022.
Available online with free registration . Last accessed April 11, 2023. - Lauver D, Ho CH: Explaining delay in care seeking for breast cancer symptoms. J Appl Soc Psychol 23 (21): 1806-25, 1993.
- MacFarlane ME, Sony SD: Women, breast lump discovery, and associated stress. Health Care Women Int 13 (1): 23-32, 1992 Jan-Mar.
- Gram IT, Slenker SE: Cancer anxiety and attitudes toward mammography among screening attenders, nonattenders, and women never invited. Am J Public Health 82 (2): 249-51, 1992.
- Lerman C, Kash K, Stefanek M: Younger women at increased risk for breast cancer: perceived risk, psychological well-being, and surveillance behavior. J Natl Cancer Inst Monogr (16): 171-6, 1994.
- Velikova G, Selby PJ, Snaith PR, et al.: The relationship of cancer pain to anxiety. Psychother Psychosom 63 (3-4): 181-4, 1995.
- Glover J, Dibble SL, Dodd MJ, et al.: Mood states of oncology outpatients: does pain make a difference? J Pain Symptom Manage 10 (2): 120-8, 1995.
- Ferrell-Torry AT, Glick OJ: The use of therapeutic massage as a nursing intervention to modify anxiety and the perception of cancer pain. Cancer Nurs 16 (2): 93-101, 1993.
- Davis-Ali SH, Chesler MA, Chesney BK: Recognizing cancer as a family disease: worries and support reported by patients and spouses. Soc Work Health Care 19 (2): 45-65, 1993.
- Dahlquist LM, Czyzewski DI, Copeland KG, et al.: Parents of children newly diagnosed with cancer: anxiety, coping, and marital distress. J Pediatr Psychol 18 (3): 365-76, 1993.
- Payne SA: A study of quality of life in cancer patients receiving palliative chemotherapy. Soc Sci Med 35 (12): 1505-9, 1992.
- Nakamura ZM, Deal AM, Nyrop KA, et al.: Serial Assessment of Depression and Anxiety by Patients and Providers in Women Receiving Chemotherapy for Early Breast Cancer. Oncologist 26 (2): 147-156, 2021.
Definitions
To effectively match patient needs with treatment interventions, health care professionals must be able to distinguish the periodic difficulties that characterize normal adjustment from more-serious mental disorders. To assist in this evaluation, health care professionals need to understand the distinctions among a variety of related concepts, as defined below.
Normal adjustment: Adjustment or psychosocial adaptation to cancer has been defined as an ongoing process in which the individual patient tries to manage emotional distress, solve specific cancer-related problems, and gain mastery of or control over cancer-related life events.[
Psychosocial distress: Distress in cancer has been defined as "a multifactorial unpleasant experience of a psychological (i.e., cognitive, behavioral, emotional), social, spiritual, and/or physical nature that may interfere with one's ability to cope effectively with cancer, its physical symptoms, and its treatment. Distress extends along a continuum, ranging from common normal feelings of vulnerability, sadness, and fears to problems that can become disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis."[
Adjustment disorders: The adjustment disorders, a diagnostic category of the fifth edition of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-5),[
Anxiety disorders: Anxiety disorders are a group of mental disorders whose common symptoms include excessive anxiety, worry, fear, apprehension, and/or dread. Although some anxiety can be adaptive—particularly in response to stressors such as cancer—anxiety disorders are excessive, unwarranted, often illogical fears, worry, and dread. The DSM-5 includes generalized anxiety disorder, panic disorder, agoraphobia, social anxiety disorder, specific phobia, obsessive-compulsive disorder, and post-traumatic stress disorder as types of anxiety disorders.[
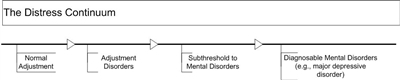
The distress continuum. Psychosocial distress exists on a continuum that ranges from normal adjustment issues to syndromes that meet the full diagnostic criteria for a mental disorder.
References:
- Brennan J: Adjustment to cancer - coping or personal transition? Psychooncology 10 (1): 1-18, 2001 Jan-Feb.
- Folkman S, Greer S: Promoting psychological well-being in the face of serious illness: when theory, research and practice inform each other. Psychooncology 9 (1): 11-9, 2000 Jan-Feb.
- Nicholas DR, Veach TA: The psychosocial assessment of the adult cancer patient. Prof Psychol 31 (2): 206-15, 2000.
- National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology: Distress Management. Version 2.2023. Plymouth Meeting, Pa: National Comprehensive Cancer Network, 2022.
Available online with free registration . Last accessed April 11, 2023. - Fashoyin-Aje LA, Martinez KA, Dy SM: New patient-centered care standards from the commission on cancer: opportunities and challenges. J Support Oncol 10 (3): 107-11, 2012 May-Jun.
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association, 2013.
Risk Factors: Prevalence and Predictors of Distress
A few studies have investigated the prevalence of distress as measured by the National Comprehensive Cancer Network Distress Thermometer (DT) or other screening instruments, such as the Brief Symptom Inventory (BSI).[
Pooled results from multiple studies suggest that approximately 40% of cancer patients report significant distress.[
- Disability.
- Poorer quality of life.
- Ongoing, unmet psychosocial needs.
In regard to prevalence of distress along the clinical course, one study of 236 women newly diagnosed with breast cancer (awaiting their initial consultation with a surgical oncologist) found that 41% reported distress scores higher than 5 on the DT. In this same group of women, 11% reported symptoms suggestive of major depression, and 10% reported symptoms of post-traumatic stress.[
Regarding predictors of distress, in a large sample (N = 380) of patients with mixed cancer diagnoses, those reporting a score of 4 or higher on the DT were more likely to be women; to have poorer functional performance (self-reported Karnofsky Performance Scale); and to have reported (on a problem checklist that accompanies the DT) problems with housing, dealing with children, dealing with a partner, depression, fears, nervousness, sadness, worry, and 14 of 20 physical ailments.[
In regard to predictors of posttreatment distress, a longitudinal study of 224 patients with head and neck cancer found that participants were more likely to experience an anxiety disorder immediately posttreatment when they were diagnosed with advanced-stage cancer or had experienced childhood abuse.[
- Younger age.
- Non-White racial status.
- Less formal education.
Clinical variables associated with posttreatment distress included the following:
- Having a mastectomy rather than lumpectomy.
- Receiving hormonal treatment.
- The presence of a diagnosable mental disorder at the time of recruitment into the study.
A comprehensive analysis of prospective studies investigated predictors of longer-term distress (≥12 months from the time of diagnosis).[
References:
- Hoffman BM, Zevon MA, D'Arrigo MC, et al.: Screening for distress in cancer patients: the NCCN rapid-screening measure. Psychooncology 13 (11): 792-9, 2004.
- Jacobsen PB, Donovan KA, Trask PC, et al.: Screening for psychologic distress in ambulatory cancer patients. Cancer 103 (7): 1494-502, 2005.
- Akizuki N, Akechi T, Nakanishi T, et al.: Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer 97 (10): 2605-13, 2003.
- Cook SA, Salmon P, Hayes G, et al.: Predictors of emotional distress a year or more after diagnosis of cancer: A systematic review of the literature. Psychooncology 27 (3): 791-801, 2018.
- Syrowatka A, Motulsky A, Kurteva S, et al.: Predictors of distress in female breast cancer survivors: a systematic review. Breast Cancer Res Treat 165 (2): 229-245, 2017.
- Trask PC, Paterson A, Riba M, et al.: Assessment of psychological distress in prospective bone marrow transplant patients. Bone Marrow Transplant 29 (11): 917-25, 2002.
- Carlson LE, Waller A, Mitchell AJ: Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol 30 (11): 1160-77, 2012.
- Hegel MT, Moore CP, Collins ED, et al.: Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer 107 (12): 2924-31, 2006.
- Henry M, Sargi E, Frenkiel S, et al.: Longitudinal study indicating antecedent psychosocial vulnerability as predictor of anxiety disorders post-treatment in people with head and neck cancer. Psychooncology 30 (11): 1910-1919, 2021.
- Jim HS, Andrykowski MA, Munster PN, et al.: Physical symptoms/side effects during breast cancer treatment predict posttreatment distress. Ann Behav Med 34 (2): 200-8, 2007 Sep-Oct.
Screening and Assessment
Screening and assessment have been viewed as two distinct processes.[
Self-Report Screening Instruments
Studies have tested the ability of single-item measures to accurately identify patients in distress.[
The Distress Thermometer (DT)
The DT, the National Comprehensive Cancer Network (NCCN) single-item and rapid-screening instrument, asks patients to rate their distress on a scale of 0 to 10, with 10 being extreme distress. On an accompanying checklist, patients are asked to indicate what has been a problem for them in the past week.[
The DT was found to have reasonable convergent and divergent validity when compared with two well-established, multidimensional symptom inventories. This very brief rapid-screening procedure has a moderate ability to accurately detect distress, as defined by scores indicative of caseness on the two-symptom inventories. In a systematic review and meta-analysis of 42 studies of distress in people with heterogenous cancer types, a DT cutoff score of 4 or higher was found to maximize the sensitivity and specificity of the measure for identifying distress.[
Other self-report screening instruments
Many other self-report questionnaires have been used as screening instruments (see Table 1); in general, they also are better for ruling out distress and perform poorly at confirming distress. Thus, most screening instruments will yield a high number of false-positive results and need to be followed by a more-extensive psychosocial assessment interview.
| Title | Items (no.) | Time (min) | Constructs Measured |
|---|---|---|---|
| Brief Symptom Inventory (BSI)[ |
53 | 7–10 | Somatization, anxiety, interpersonal sensitivity, depression, hostility, phobic anxiety, paranoid ideation, psychoticism, and obsessive-compulsiveness |
| Brief Symptom Inventory (BSI-18)[ |
18 | 3–5 | Somatization, depression, anxiety, and general distress |
| Distress Thermometer (DT) and Problem List[ |
Varies | 2–3 | Distress and problems related to the distress |
| Functional Assessment of Chronic Illness Therapy (FACIT; formerly the Functional Assessment of Cancer Therapy [FACT])[ |
27 | 5–10 | 4 domains of quality of life: physical, functional, social/family, and emotional well-being |
| Hospital Anxiety and Depression Scale (HADS)[ |
14 | 5–10 | Emotional-cognitive symptoms of clinical depression and anxiety without neurovegetative symptoms |
| Patient-Reported Outcomes Measurement Information System (PROMIS) screeners[ |
Up to 88 (8–15 per domain) | Varies | Clinical norms based on age, cancer stage, and cancer type across 8 domains (anxiety, depression, pain interference, fatigue, sleep disturbance, physical functioning, social functioning, and cognitive functioning); each domain can be given separately |
| Profile of Mood States (POMS)[ |
65 | 10–25 | 6 mood states: anxiety, fatigue, confusion, depression, anger, and vigor |
| Zung Self-Rating Depression Scale[ |
20 | 5–10 | Symptoms of depression |
Self-report screening instruments must be scored, evaluated, and discussed with each patient. Triage—the process of communicating screening results, discussing each patient's needs, and determining the best course of further action—is key to the successful use of screening. In fact, screening without availability of appropriate treatment resources is considered unethical. The primary oncology team (oncologist, nurse, palliative care specialist, social worker, and counselor) is responsible for successful triage. In some studies, a significant percentage of patients who report moderate to high levels of distress refuse further assessment.[
The NCCN standards of care [
Psychosocial Assessment
The assessment of psychosocial adaptation should follow screening when distress is identified. The psychosocial assessment is typically a semistructured interview during which the professional evaluates how well an individual patient, a patient's family, and other significant people in a patient's life are adapting to the current demands of the illness. In general, this assessment process considers a wide variety of factors relevant to overall adaptation.[
A successful transition from screening to assessment involves clear communication between the oncology team and the patient. Although there is no single best way to talk to patients about psychosocial needs, clinical experience suggests some important concepts. First, most patients will respond to the recommendations of health care professionals who exhibit trust, expertise, warmth, care, and concern.
Choice of words is important. Words that suggest the stigma of serious mental illness, such as psychiatric, psychological, mental disorder, maladjustment, or mental illness, should be avoided—in favor of words such as distress, concerns, worries, uncertainties, or stressors from the illness or its treatment. Suggestions for word choice include the following:
- The questionnaire you filled out helps us to understand you as a whole person, and we want to provide the best care possible for you—physically, emotionally, socially, and spiritually.
- As you may realize, a serious illness can affect the quality of your life in many ways (emotionally, socially, financially, and in regard to work, relationships, and energy). There is much more to this illness than just the physical, and we want to be sure we are addressing these other dimensions of your life.
- Your concerns and worries are very understandable, given your illness and its treatment. We do not want to ignore the (emotional, social, spiritual) aspects of your experience right now.
- We have found that many patients benefit greatly from a chance to talk further about their concerns with a health care professional (e.g., social worker, mental health professional, palliative care specialist, or pastoral counselor), and we would like to schedule that for you.
- For further explanation, we suggest an interview that lasts about 45 minutes with a professional who will:
- Listen closely to you.
- Want to know about your experiences with your illness.
- Ask about you, your family and friends, and other support persons.
- Ask about how you have been adjusting to your illness and may encourage you to continue (and give you feedback about) successful coping strategies you are already using.
- Suggest additional ways to address your concerns.
Model Screening Programs
Various comprehensive cancer centers have developed models for screening for psychosocial distress. Although there are notable differences, most models involve the following sequential steps:
- Screening administration.
- Scoring and evaluation.
- Referral.
Most screening for psychosocial distress focuses on the individual patient; however, some family-focused screening procedures are being developed.[
Administration of a screening instrument involves a 5- to 10-minute process in which each patient answers a series of simple, straightforward questions about distress, either orally or via a self-report paper or computer questionnaire. Answers are scored and evaluated on the basis of previously determined criteria. If scores fall above the defined criteria, then a formal referral to the appropriate discipline (social work, psychology, psychiatry, palliative care, or pastoral care) is made. Distress management then begins with a more-comprehensive face-to-face psychosocial assessment interview [
The success of screening programs can be measured in terms of the following outcomes:
- Accurate identification of patients who are experiencing significant psychosocial distress.
- Improved referral of patients to appropriate health care professionals to address clinically relevant distress.
- Acceptance of such referrals by patients who are experiencing high-level distress.
- Improved patient-clinician communication, with frequent discussion of quality-of-life issues during patient visits.
- Decreased level of distress and improved quality of life resulting from the screening program.
Few empirical studies have evaluated the impact of structured screening programs using these outcomes. In most of these studies, intervention included telephone follow-up of screening results with referrals or in-person discussions with clinicians, trained or untrained in screening. Study designs have differed in terms of screening tools (brief vs. comprehensive screening tools), intervention components (trained vs. untrained screening clinicians), and study outcomes. Study designs have also differed in their controls; for example, control groups in some studies did not undergo screening,[
The results of the screening studies have been mixed, depending on the structure of the screening programs and the assessed outcomes. Two studies found no meaningful differences between control and intervention groups in distress, quality of life, or cancer needs.[
In one study, a subgroup of moderately to severely depressed patients showed a significant reduction in depression after the intervention,[
Given these mixed results, further empirical evaluation of the effectiveness of screening programs is necessary. The following examples will help to illustrate the process.
Memorial Sloan-Kettering Cancer Center has experimented with the DT, which was modeled after tools used to measure pain.[
- No distress at a rating of 0.
- Extreme distress at a rating of 10.
Patients are asked to rate the distress they have been experiencing in the past week, including the day of the screening, on a scale of 0 to 10. Accompanying the DT is a problem checklist that helps identify relevant potential sources of stress. The patient is asked to check the problems that are most relevant. Categories of problems include the following:
- Practical (e.g., housing, insurance, or transportation).
- Physical (e.g., pain, nausea, or fatigue).
- Family or support (e.g., partner, children, or friends).
- Emotional (e.g., worry, sadness, depression, or anger).
- Spiritual/religious (e.g., relating to God or loss of faith).
The primary oncology team (oncologist, nurse, palliative care specialist, and social worker) is responsible for administering this brief screening, evaluating a patient's response, and arranging for a referral, when necessary. Preliminary testing of this procedure used a cutoff score of 4 or higher as requiring further evaluation. Initial needs assessments have shown that 20% to 52% of patients report significant levels of distress.[
At Johns Hopkins Cancer Center, all new patients receive an 18-item version of the Brief Symptom Inventory (BSI),[
The Oncology Symptom Control Research group at Community Cancer Care typically screens all incoming patients with the Zung Self-Rating Depression Scale (ZSDS).[
References:
- Nicholas DR, Veach TA: The psychosocial assessment of the adult cancer patient. Prof Psychol 31 (2): 206-15, 2000.
- Zabora JR: Screening procedures for psychosocial distress. In: Holland JC, Breitbart W, Jacobsen PB, et al., eds.: Psycho-oncology. Oxford University Press, 1998, pp 653-61.
- Zabora JR, Smith-Wilson R, Fetting JH, et al.: An efficient method for psychosocial screening of cancer patients. Psychosomatics 31 (2): 192-6, 1990 Spring.
- Hoffman BM, Zevon MA, D'Arrigo MC, et al.: Screening for distress in cancer patients: the NCCN rapid-screening measure. Psychooncology 13 (11): 792-9, 2004.
- Jacobsen PB, Donovan KA, Trask PC, et al.: Screening for psychologic distress in ambulatory cancer patients. Cancer 103 (7): 1494-502, 2005.
- Akizuki N, Akechi T, Nakanishi T, et al.: Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer 97 (10): 2605-13, 2003.
- Dabrowski M, Boucher K, Ward JH, et al.: Clinical experience with the NCCN distress thermometer in breast cancer patients. J Natl Compr Canc Netw 5 (1): 104-11, 2007.
- Keir ST, Calhoun-Eagan RD, Swartz JJ, et al.: Screening for distress in patients with brain cancer using the NCCN's rapid screening measure. Psychooncology 17 (6): 621-5, 2008.
- National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology: Distress Management. Version 2.2023. Plymouth Meeting, Pa: National Comprehensive Cancer Network, 2022.
Available online with free registration . Last accessed April 11, 2023. - Ma X, Zhang J, Zhong W, et al.: The diagnostic role of a short screening tool--the distress thermometer: a meta-analysis. Support Care Cancer 22 (7): 1741-55, 2014.
- Riba MB, Donovan KA, Andersen B, et al.: Distress Management, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 17 (10): 1229-1249, 2019.
- Patterson P, D'Agostino NM, McDonald FEJ, et al.: Screening for distress and needs: Findings from a multinational validation of the Adolescent and Young Adult Psycho-Oncology Screening Tool with newly diagnosed patients. Psychooncology 30 (11): 1849-1858, 2021.
- Derogatis LR, Melisaratos N: The Brief Symptom Inventory: an introductory report. Psychol Med 13 (3): 595-605, 1983.
- Derogatis LR: BSI-18: Brief Symptom Inventory 18. Administration, Scoring and Procedures Manual. NCS Pearson, 2001.
- Hegel MT, Collins ED, Kearing S, et al.: Sensitivity and specificity of the Distress Thermometer for depression in newly diagnosed breast cancer patients. Psychooncology 17 (6): 556-60, 2008.
- Webster K, Cella D, Yost K: The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes 1: 79, 2003.
- Kugaya A, Akechi T, Okuyama T, et al.: Prevalence, predictive factors, and screening for psychologic distress in patients with newly diagnosed head and neck cancer. Cancer 88 (12): 2817-23, 2000.
- Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand 67 (6): 361-70, 1983.
- Love AW, Kissane DW, Bloch S, et al.: Diagnostic efficiency of the Hospital Anxiety and Depression Scale in women with early stage breast cancer. Aust N Z J Psychiatry 36 (2): 246-50, 2002.
- Jensen RE, Potosky AL, Moinpour CM, et al.: United States Population-Based Estimates of Patient-Reported Outcomes Measurement Information System Symptom and Functional Status Reference Values for Individuals With Cancer. J Clin Oncol 35 (17): 1913-1920, 2017.
- McNair DM, Lorr M, Droppleman LF: Profile of Mood States Manual. Educational and Industrial Testing Service, 1992.
- Dugan W, McDonald MV, Passik SD, et al.: Use of the Zung Self-Rating Depression Scale in cancer patients: feasibility as a screening tool. Psychooncology 7 (6): 483-93, 1998 Nov-Dec.
- Roth AJ, Kornblith AB, Batel-Copel L, et al.: Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer 82 (10): 1904-8, 1998.
- Carroll BT, Kathol RG, Noyes R, et al.: Screening for depression and anxiety in cancer patients using the Hospital Anxiety and Depression Scale. Gen Hosp Psychiatry 15 (2): 69-74, 1993.
- Ibbotson T, Maguire P, Selby P, et al.: Screening for anxiety and depression in cancer patients: the effects of disease and treatment. Eur J Cancer 30A (1): 37-40, 1994.
- Razavi D, Delvaux N, Farvacques C, et al.: Screening for adjustment disorders and major depressive disorders in cancer in-patients. Br J Psychiatry 156: 79-83, 1990.
- Kissane DW, McKenzie M, McKenzie DP, et al.: Psychosocial morbidity associated with patterns of family functioning in palliative care: baseline data from the Family Focused Grief Therapy controlled trial. Palliat Med 17 (6): 527-37, 2003.
- Maunsell E, Brisson J, Deschênes L, et al.: Randomized trial of a psychologic distress screening program after breast cancer: effects on quality of life. J Clin Oncol 14 (10): 2747-55, 1996.
- McLachlan SA, Allenby A, Matthews J, et al.: Randomized trial of coordinated psychosocial interventions based on patient self-assessments versus standard care to improve the psychosocial functioning of patients with cancer. J Clin Oncol 19 (21): 4117-25, 2001.
- Carlson LE, Groff SL, Maciejewski O, et al.: Screening for distress in lung and breast cancer outpatients: a randomized controlled trial. J Clin Oncol 28 (33): 4884-91, 2010.
- Carlson LE, Waller A, Groff SL, et al.: Online screening for distress, the 6th vital sign, in newly diagnosed oncology outpatients: randomised controlled trial of computerised vs personalised triage. Br J Cancer 107 (4): 617-25, 2012.
- Zung WW: Depression in the normal aged. Psychosomatics 8 (5): 287-92, 1967 Sep-Oct.
- Zung WW: Factors influencing the self-rating depression scale. Arch Gen Psychiatry 16 (5): 543-7, 1967.
- Kirsh KL, Passik S, Holtsclaw E, et al.: I get tired for no reason: a single item screening for cancer-related fatigue. J Pain Symptom Manage 22 (5): 931-7, 2001.
Normal Adjustment
Adjustment, well-being, or psychosocial adaptation to cancer has been defined [
- Manage emotional distress.
- Solve specific cancer-related problems.
- Gain mastery of or control over cancer-related life events.
Adjustment to cancer is not a unitary, single event but rather a series of ongoing coping responses to the multiple tasks associated with living with cancer. Patients face many challenges that vary with the clinical course of the disease. Common periods of crisis and significant challenge include:
- Initial diagnosis.
- Active treatment (surgery, radiation, and chemotherapy).
- Posttreatment and remission.
- Recurrence.
- Terminating curative treatment.
- Long-term survivorship.
Each of these events may include significant challenges:
- Certain coping tasks.
- Particular existential questions.
- Common emotional responses.
- Specific problems.
Normal or successful adjustment is indicated in patients who are able to minimize disruptions to life roles, regulate emotional distress, and remain actively involved in aspects of life that continue to hold meaning and importance.
Coping refers to the specific thoughts and behaviors that patients use in their efforts to adjust.[
- Is this event personally significant to me?
- What resources do I have to manage/control this event?
A low level of distress is the result of a perception that either the demands of a situation are very low or the individual's resources are substantial.[
Coping strategies refer to specific cognitive and behavioral activities that use situation-specific coping efforts, such as readjusting one's daily routine or work schedule to adjust to the side effects of cancer treatment. Coping strategies comprise efforts to adjust. Among many successful coping strategies, three broad categories have been noted:[
- Problem focused.
- Emotion focused.
- Meaning focused.
Patients may switch among these strategies, even from adaptive to maladaptive, depending on their current functioning levels.
Problem-focused strategies help patients manage specific problems by directly trying to alter problematic situations. Some of these approaches may be adaptive (e.g., seeking information about treatment option survival rates), but some may not (e.g., paying large amounts of money for unproven treatment options).[
Emotion-focused strategies allow patients to regulate their degree of emotional distress with either emotion-engaging behaviors (e.g., seeking social support) or emotion-avoidant behaviors, as the person attempts to escape reminders of the cause of distress (e.g., not seeking treatment after a diagnosis, use of alcohol or other drugs).
Meaning-focused strategies help patients understand why an event has happened and what impact cancer will have on their lives. In general, people who adjust well typically remain committed to and actively engaged in the process of coping with cancer and continue to find meaning and importance in their lives. People who do not adjust well often withdraw, become disengaged, and feel hopeless. Thus, assessing the degree of engagement versus giving up may be a way to distinguish between successful and unsuccessful adjustment.
Coping style refers to the most-common, more-frequent, and longer-term use of a set of coping strategies (e.g., use of alcohol, seeking social support, use of religious/spirituality resources) that an individual tends to use across a variety of life situations. Coping style is often closely related to overall disposition and personality (e.g., optimism, pessimism, introversion, extroversion).[
One criticism of the literature on coping with cancer focuses on the assumption that coping with cancer is a unitary, single event. In reality, coping with cancer involves coping styles and strategies that may vary according to the nature of the stressors being encountered. For example, in a study of 52 adults receiving palliative care for cancer,[
General Factors Influencing Adjustment
Although there are some commonalities in normal adjustment to the varying stressors of cancer, there are also many individual differences. It is difficult to predict how a given patient will cope with cancer, so it is important to recognize factors that influence adjustment to cancer. One study of women with stage II or stage III breast cancer [
Another study evaluated women with stage 0 to stage III breast cancer (N = 89) at three time points: during treatment, 3 weeks following the end of treatment, and 3 months posttreatment. Most survivors showed good adjustment on general distress indices. The factors predicting sustained distress included younger age, history of depression or anxiety, and more-extensive treatment.[
Psychosocial adjustment/adaptation is influenced by three broad categories of factors:[
- Cancer derived.
- Patient derived.
- Society derived.
The personality traits of optimism and pessimism might play a critical role in the psychological well-being of cancer patients. A German study investigated the impact of optimism and pessimism on psychological well-being in 161 newly diagnosed cancer patients with heterogeneous cancers.[
The availability of social support has been found to be related to mortality from breast cancer. In a longitudinal study of 2,835 female nurses with breast cancer, those who reported no close contacts (e.g., relatives, friends, or living children) before their diagnosis had a twofold increased risk of mortality from breast cancer, compared with those who had more social contacts (e.g., ten or more close relatives).[
Situation-Specific Influences on Adjustment
Hearing the diagnosis
The process of adjusting to cancer can begin even before a diagnosis. Patients may respond with normal levels of fear, worry, and concern when they have unexplained symptoms or when they realize that they are undergoing testing to determine the presence of cancer. When they hear the diagnosis, their fears become realized, generating a psychological and existential plight (crisis).[
Active treatment
Longer-term adaptation consists of the extended time during which more long-lasting and permanent adjustment occurs. This period consists of weeks and months during which patients use a variety of coping strategies and styles. This combination of longer-term coping styles and short-term coping strategies usually serves patients well in their efforts at adaptation.[
Posttreatment remission
The completion of active treatment can cause ambivalence for cancer patients and their families. The completion of active treatment can be a time of heightened distress,[
Other adjustment issues include living with uncertainty, returning to previous life roles, and hypervigilance to health concerns, especially if the cognitive or physical effects of cancer or treatment linger.[
Normal anxiety and worry often intensify as the dates of follow-up appointments approach. Normal anxiety comes from concerns about recurrence and the related emotional consequences (e.g., re-entry into the patient role and renewed feelings of loss of control). Many patients find waiting for test results to be a particularly distressing experience.
For most individuals, this normal escalation of distress after treatment ends appears to be temporary and resolves within a few weeks. In an empirical study of posttreatment adjustment, 94 women with stage 0, I, II, or III breast cancer who were completing radiation therapy were assessed on measures of depression, anxiety, and quality of life on the last day of treatment and at 2 weeks, 4 to 6 weeks, 3 months, and 6 months posttreatment. Results found elevated symptoms of depression, low-level anxiety, and diminished quality of life on the last day of treatment; however, by 2 weeks later, symptoms of depression decreased significantly, and quality of life improved significantly.[
Recurrence
Recurrence of cancer after treatment can escalate stress for patients and may prompt providers to screen for psychosocial-spiritual distress. In a study of women with recurrent breast cancer, significant impairments in physical, functional, and emotional well-being were found within 1 month after recurrence; however, the following had positive effects on quality of life:[
- A patient's self-efficacy (confidence in the ability to manage the demands of illness).
- Social support.
- Family hardiness (family's internal strength and ability to manage hardship and change).
Conversely, the following were associated with a lower quality of life:[
- More distress about physical symptoms.
- Additional life concerns.
- A sense of hopelessness.
- A negative perception of illness or caregiving.
The patient who successfully adjusts to the crisis of recurrence often shifts expectations and maintains hope through a variety of meaningful life activities. For example, a patient who has confidence that pain and suffering can be controlled will have hope for future quality of life. Religion and spirituality also play an important role in helping many patients maintain mental and physical quality of life. As with screening for physical and mental health conditions that may interfere with quality of life, providers may wish to screen for spiritual health as part of the adjustment to this stage of cancer to make appropriate referrals.[
Advanced cancer and noncurative treatment
Patients with advanced cancer may experience psychological distress, physical symptoms, and the existential crisis of death, all of which may combine to result in significant suffering.[
How patients with advanced cancer perceive their prognosis may be one reason for psychosocial distress. In a cross-sectional, descriptive study of 559 patients with incurable cancer, patients completed the Prognosis and Treatment Perception Questionnaire and the Hospital Anxiety and Depression Scale (HADS).[
- About 62% of participants reported that both their and their oncologist's treatment goals were noncurative. Of these participants, 27% reported depression and 32% reported anxiety.
- Nineteen percent of participants reported that both their and their oncologist's treatment goals were curative, of whom 19% reported depression and 23% reported anxiety.
- Fourteen percent of participants reported that their goal was curative treatment and their oncologist's goal was noncurative care, of whom 27% reported depression and 37% reported anxiety.
- Five percent of participants reported that their goal was noncurative care and their oncologist's goal was curative treatment, of whom 21% reported depression and 39% reported anxiety.
The findings of this study suggest that patients with discordant perceptions of their treatment goal and their oncologist's treatment goal may be more likely to experience anxiety. An important limitation of this study is that the authors did not assess clinicians' treatment goals or patients' treatment status. In addition, the study was conducted at a single cancer center with a predominantly White, non-Hispanic sample. Nevertheless, the findings highlight the importance of patient-centered communication and psychosocial support, particularly when discussing goals of care. For more information, see Communication in Cancer Care.
Long-term survivorship
The adjustment from posttreatment to long-term survivorship is gradual and extends over many years. However, most patients, despite various cancer diagnoses and treatments, adjust well, with some even reporting benefits to a cancer diagnosis (e.g., greater appreciation of life, reprioritizing of life values, strengthening of spiritual or religious beliefs).[
- Greater medical problems.
- Fewer social supports.
- Poorer premorbid psychological adjustment.
- Fewer economic resources.
In general, studies of cancer survivors and healthy comparison groups have found no significant differences in measures of psychological distress, marital and sexual adjustment, social functioning, and overall psychosocial functioning.
However, many cancer patients experience some common areas of distress that are subthreshold or not severe enough to meet diagnostic criteria, including:[
- Anxiety about recurrence.
- An increased sense of vulnerability.
- Lowered sense of control.
- Conditioned reminders of chemotherapy (smells, sights) that produce anxiety and nausea.
- Post-traumatic stress–like symptoms (such as persistent, intrusive thoughts or recurrent imagery associated with cancer).
- Fatigue.
- Concerns about body image and sexuality.
An assessment of more than 6,000 cancer survivors found that more than 50% reported fear of recurrence, mostly with low intensity. Survivors at risk of experiencing high levels of fear of recurrence included women survivors, individuals younger than 59 years, those at 5 to 7 years postdiagnosis, socially isolated individuals, those with lower education levels, and individuals with a history of metastases or recurrence.[
In one of the few prospective longitudinal studies of cancer survivors, 752 patients from three U.S. states were asked about a variety of psychosocial problems. About 1 year after diagnosis, 68% felt fearful that their illness would return, approximately 60% were concerned about relapsing, and 58% had fears about the future. In addition, approximately two out of three survivors were concerned about a physical health problem, such as fatigue and loss of strength. Approximately 48% reported sleep difficulties, and 41% reported concerns with sexual dysfunction. Younger survivors (aged 18–54 years), women, non-White patients, unmarried survivors, and those with lower incomes reported more problems. In comparisons of four common cancers, the most concerns regarding problems in living were reported by those with lung cancer, followed by survivors of breast, colorectal, and prostate cancers.[
Referral to psycho-oncology services may benefit patients during survivorship. A prospective observational study of 243 adults referred for psycho-oncology services assessed the impact of one or two visits for pharmacotherapy and/or psychotherapy on depression and distress.[
Multifocal interventions may help cancer survivors address multiple mental and physical health issues simultaneously. In a multicenter trial of 222 posttreatment breast cancer survivors, researchers implemented the Better Exercise Adherence after Treatment for Cancer (BEAT Cancer) intervention. In this study, over 3 months, patients engaged in 12 supervised exercise sessions that were tapered to an unsupervised at-home exercise program (though logged with a heart rate monitor), individual counseling sessions, and group counseling. These sessions encouraged regular exercise, promoted self-monitoring, and engaged patients in cognitive reframing of current physical limitations, which had a significant positive impact on body image, mood, cardiovascular fitness, and general quality of life.[
A large (N = 660) longitudinal study of women breast cancer survivors older than 65 years investigated factors associated with changes in emotional well-being. Overall findings suggested that the 5-year survivorship experience for most women is relatively stable, with few changes in emotional well-being. However, women who had fewer than 12 years of formal education and women who perceived themselves as never being cured were more likely to experience declines in emotional well-being, while those who had better physical functioning, good emotional support, and the perception of positive physician-patient communication were less likely to have poor emotional health.[
References:
- Brennan J: Adjustment to cancer - coping or personal transition? Psychooncology 10 (1): 1-18, 2001 Jan-Feb.
- Folkman S, Greer S: Promoting psychological well-being in the face of serious illness: when theory, research and practice inform each other. Psychooncology 9 (1): 11-9, 2000 Jan-Feb.
- Nicholas DR, Veach TA: The psychosocial assessment of the adult cancer patient. Prof Psychol 31 (2): 206-15, 2000.
- Lazarus RS, Folkman S: Stress, Appraisal, and Coping. Springer Publishing Co, 1984.
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association, 2013.
- Pearlin LI, Schooler C: The structure of coping. J Health Soc Behav 19 (1): 2-21, 1978.
- Ahmad MM, Musil CM, Zauszniewski JA, et al.: Prostate cancer: appraisal, coping, and health status. J Gerontol Nurs 31 (10): 34-43, 2005.
- Ransom S, Jacobsen PB, Schmidt JE, et al.: Relationship of problem-focused coping strategies to changes in quality of life following treatment for early stage breast cancer. J Pain Symptom Manage 30 (3): 243-53, 2005.
- Schou I, Ekeberg Ø, Ruland CM, et al.: Pessimism as a predictor of emotional morbidity one year following breast cancer surgery. Psychooncology 13 (5): 309-20, 2004.
- De Faye BJ, Wilson KG, Chater S, et al.: Stress and coping with advanced cancer. Palliat Support Care 4 (3): 239-49, 2006.
- Golden-Kreutz DM, Thornton LM, Wells-Di Gregorio S, et al.: Traumatic stress, perceived global stress, and life events: prospectively predicting quality of life in breast cancer patients. Health Psychol 24 (3): 288-96, 2005.
- Costanzo ES, Lutgendorf SK, Mattes ML, et al.: Adjusting to life after treatment: distress and quality of life following treatment for breast cancer. Br J Cancer 97 (12): 1625-31, 2007.
- Pinquart M, Fröhlich C, Silbereisen RK: Optimism, pessimism, and change of psychological well-being in cancer patients. Psychol Health Med 12 (4): 421-32, 2007.
- Kroenke CH, Kubzansky LD, Schernhammer ES, et al.: Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol 24 (7): 1105-11, 2006.
- Weisman AD, Worden JW: The existential plight in cancer: significance of the first 100 days. Int J Psychiatry Med 7 (1): 1-15, 1976-77.
- Bishop SJ: Trait anxiety and impoverished prefrontal control of attention. Nat Neurosci 12 (1): 92-8, 2009.
- Visser MR, van Lanschot JJ, van der Velden J, et al.: Quality of life in newly diagnosed cancer patients waiting for surgery is seriously impaired. J Surg Oncol 93 (7): 571-7, 2006.
- Paek MS, Ip EH, Levine B, et al.: Longitudinal Reciprocal Relationships Between Quality of Life and Coping Strategies Among Women with Breast Cancer. Ann Behav Med 50 (5): 775-783, 2016.
- Bryant AL, Smith SK, Zimmer C, et al.: An exploratory path model of the relationships between positive and negative adaptation to cancer on quality of life among non-Hodgkin lymphoma survivors. J Psychosoc Oncol 33 (3): 310-31, 2015.
- Oppegaard K, Harris CS, Shin J, et al.: Anxiety profiles are associated with stress, resilience and symptom severity in outpatients receiving chemotherapy. Support Care Cancer 29 (12): 7825-7836, 2021.
- Henselmans I, Helgeson VS, Seltman H, et al.: Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol 29 (2): 160-8, 2010.
- Sherman AC, Simonton S: Family therapy for cancer patients: clinical issues and interventions. The Family Journal: Counseling and Therapy for Couples and Families 7 (1): 39-50, 1999.
- Helgeson VS, Snyder P, Seltman H: Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change. Health Psychol 23 (1): 3-15, 2004.
- Deshields T, Tibbs T, Fan MY, et al.: Ending treatment: the course of emotional adjustment and quality of life among breast cancer survivors immediately following radiation therapy. Support Care Cancer 13 (12): 1018-26, 2005.
- Northouse LL, Mood D, Kershaw T, et al.: Quality of life of women with recurrent breast cancer and their family members. J Clin Oncol 20 (19): 4050-64, 2002.
- Kristeller JL, Rhodes M, Cripe LD, et al.: Oncologist Assisted Spiritual Intervention Study (OASIS): patient acceptability and initial evidence of effects. Int J Psychiatry Med 35 (4): 329-47, 2005.
- Ray A, Block SD, Friedlander RJ, et al.: Peaceful awareness in patients with advanced cancer. J Palliat Med 9 (6): 1359-68, 2006.
- Cherny NI, Coyle N, Foley KM: Suffering in the advanced cancer patient: a definition and taxonomy. J Palliat Care 10 (2): 57-70, 1994 Summer.
- Mitchell AJ, Chan M, Bhatti H, et al.: Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 12 (2): 160-74, 2011.
- El-Jawahri A, Forst D, Fenech A, et al.: Relationship Between Perceptions of Treatment Goals and Psychological Distress in Patients With Advanced Cancer. J Natl Compr Canc Netw 18 (7): 849-855, 2020.
- Polinsky ML: Functional status of long-term breast cancer survivors: demonstrating chronicity. Health Soc Work 19 (3): 165-73, 1994.
- Curbow B, Somerfield MR, Baker F, et al.: Personal changes, dispositional optimism, and psychological adjustment to bone marrow transplantation. J Behav Med 16 (5): 423-43, 1993.
- Belec RH: Quality of life: perceptions of long-term survivors of bone marrow transplantation. Oncol Nurs Forum 19 (1): 31-7, 1992 Jan-Feb.
- Tartaro J, Roberts J, Nosarti C, et al.: Who benefits?: distress, adjustment and benefit-finding among breast cancer survivors. J Psychosoc Oncol 23 (2-3): 45-64, 2005.
- Smith MY, Redd WH, Peyser C, et al.: Post-traumatic stress disorder in cancer: a review. Psychooncology 8 (6): 521-37, 1999 Nov-Dec.
- Koch-Gallenkamp L, Bertram H, Eberle A, et al.: Fear of recurrence in long-term cancer survivors-Do cancer type, sex, time since diagnosis, and social support matter? Health Psychol 35 (12): 1329-1333, 2016.
- Baker F, Denniston M, Smith T, et al.: Adult cancer survivors: how are they faring? Cancer 104 (11 Suppl): 2565-76, 2005.
- Molinaro J, Banerjee A, Lyndon S, et al.: Reducing distress and depression in cancer patients during survivorship. Psychooncology 30 (6): 962-969, 2021.
- Rogers LQ, Courneya KS, Anton PM, et al.: Effects of a multicomponent physical activity behavior change intervention on fatigue, anxiety, and depressive symptomatology in breast cancer survivors: randomized trial. Psychooncology 26 (11): 1901-1906, 2017.
- Clough-Gorr KM, Ganz PA, Silliman RA: Older breast cancer survivors: factors associated with change in emotional well-being. J Clin Oncol 25 (11): 1334-40, 2007.
Psychosocial Distress
Distress in cancer has been defined as "a multifactorial unpleasant experience of a psychological (i.e., cognitive, behavioral, emotional), social, spiritual, and/or physical nature that may interfere with one's ability to cope effectively with cancer, its physical symptoms, and its treatment. Distress extends along a continuum, ranging from common normal feelings of vulnerability, sadness, and fears to problems that can become disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis."[
The broad goal of the National Comprehensive Cancer Network (NCCN) is to establish standards of care so that all patients experiencing psychosocial distress will be accurately and routinely identified, recognized, and treated promptly at all stages of disease.[
- Screening.
- Triage.
- Initial evaluation.
Also included are referral and treatment guidelines for each participating profession:
- Mental health (psychology and psychiatry).
- Social work.
- Palliative care.
- Pastoral care.
Distress and the need for screening are most likely to occur during the following periods:
- Shortly after diagnosis.
- At the start of treatment (surgery, radiation, and chemotherapy).
- At the conclusion of a long course of treatment.
- Periodically during posttreatment and remission.
- At the time of recurrence.
- With transition to palliative care.
For more information, see the Overview section.
Psychosocial Interventions for Distress
An extensive body of literature supports the efficacy of psychosocial interventions for adult cancer patients.[
Psychosocial interventions have generally been defined as nonpharmacological interventions that include a variety of psychological and educational components. Typical components include the following:
- Relaxation training.
- Cognitive and behavioral coping strategies.
- Cancer education/information sessions.
- Existential therapy.
- Group social support.
Interventions have included various combinations of these components, have varied in length (single session to multiple weekly sessions), and have been administered in both individual and group formats. The most common patient population has been U.S. White women of middle to higher socioeconomic status who have breast cancer; however, some studies included mixed cancer diagnoses, and studies from European countries have appeared.[
- Emotional adjustment (e.g., depression, anxiety).
- Functional impairment (e.g., return to work, social roles).
- Disease-related symptoms (e.g., nausea/vomiting, fatigue, pain).
- Health behaviors (e.g., diet, smoking, exercise).
- Immune system functioning.
A biobehavioral model [
Although positive benefits have been found, their clinical significance has been questioned. Reviewers have offered varying conclusions regarding the size of these positive effects,[
Effect sizes may be related to the timing of the intervention and patient selection procedures. For most patients, levels of psychosocial distress are highest during the earliest days of their cancer experience and, for many, dissipate quickly. Thus, if interventions are offered later in the cancer experience (weeks or months after diagnosis and treatment), patients may have less distress than they would have experienced if interventions had been offered earlier, making large effects more difficult to detect.[
In one study,[
- A control group that received standard disease management.
- A standardized psychoeducation group.
- A group that received telephone counseling.
- A group that received psychoeducation plus telephone counseling.
Patients and partners who received the study interventions had less side-effect distress and severity as well as higher levels of psychological well-being than did those who received standard care. In addition, the study results supported the efficacy of low-cost, replicable interventions by video and telephone to achieve these physical and psychological benefits.[
Two meta-analyses [
- 0.19 for depression [
5 ] and functional adjustment.[4 ] - 0.24 for emotional adjustment.[
4 ] - 0.26 for treatment- or disease-related symptoms.[
4 ] - 0.28 for global measures of outcome.[
4 ] - 0.36 for anxiety.[
5 ]
These positive effect sizes indicate that the average patient receiving the intervention is better off than between 57% and 65% of those not receiving the intervention.
In summary, it appears that when psychosocial interventions are offered to patients who are experiencing distress (e.g., anxiety, depression), the efficacy of the intervention is very strong. Thus, the overall positive benefit for psychosocial interventions seems to be greater with those who seem to need it most.[
Randomized trial of group interventions for breast cancer
The study described below is representative of randomized clinical trials testing the efficacy of small-group psychosocial interventions for U.S. women with early-stage breast cancer. Studies vary in total treatment time, from 8 hours [
Investigators evaluated an educational intervention consisting of 2-hour once-per-month group sessions for 4 consecutive months.[
- A standard medical care group.
- A nutrition education group.
- A psychosocial education group.
The psychosocial and nutrition education groups included information dissemination, discussion, and some activities/exercises. Topics rotated monthly, and participants could join a group at any time (i.e., they were open groups). In general, patient-to-patient interaction was minimal because sessions were more didactic presentations. The psychosocial education group presented topics relevant to younger women with breast cancer, such as the following:
- Talking with children about cancer.
- How to carry on with life after a diagnosis.
- Relationships/intimacy with partners.
- Hormones and cancer.
- Genetic bases of breast cancer.
The nutrition education group included information about choosing fruits, vegetables, and low-fat foods and how to consistently incorporate these foods into daily life. Shopping, low-fat cooking, eating out, and other related topics were presented. Results showed that patients in both intervention groups reported fewer depressive symptoms and better physical functioning at a 13-month follow-up. This study is an example of a more-targeted intervention designed for a specific patient population (younger women with breast cancer) at a specific time in their treatment course (soon after completion of active treatment).
Self-administered stress management training for chemotherapy
In a randomized trial of 411 patients diagnosed with different types of cancers,[
- Paced abdominal breathing.
- Progressive muscle relaxation with imagery.
- The use of coping self-statements.
The professional provided the patient with an audiotape of the individual session, prescribed daily practice of the three techniques, and met briefly with the patient before his or her first chemotherapy session.
In the self-administered group, a professional met with each patient for approximately 10 minutes, provided him or her with a packet of instructional materials about coping with chemotherapy, and briefly instructed the patient on their use. These materials included the same information provided to the professionally administered group plus the following:
- A 15-minute videotape.
- A 12-page booklet.
- A 35-minute relaxation audiotape.
Patients in this group were instructed to first view the videotape and then review the booklet, following its instructions for further training, practice, and use of the various techniques.
Results of this novel approach found that patients in the self-administered intervention reported significantly better physical functioning, vitality, and mental health and fewer role limitations than those reported by either of the other two groups. Patients in the professionally administered group reported no better outcomes than did patients in the traditional-care group. Costs of the self-administered group were significantly lower than those of the other two groups.
Brief orientation and tour of a medical oncology clinic
A novel intervention tested the effects of a brief (15- to 20-minute) clinic tour for new patients in a medical oncology clinic.[
- An opportunity to see the phlebotomy, nursing, and chemotherapy areas.
- The distribution of written materials about clinic hours and procedures.
- A time to ask questions.
One hundred and fifty consecutively referred patients who had a variety of cancers were randomly assigned to either the clinic orientation intervention or standard care. Intervention patients showed less anxiety, less mood disturbance, and fewer depressive symptoms at a 1-week follow-up. In addition, these patients reported more knowledge of clinic procedures, more confidence in their physicians, and higher levels of satisfaction and hope. This is an example of how even a simple, minimal intervention can have positive benefits.
Use of online information
The Comprehensive Health Enhancement Support System (CHESS) [
- Didactic material.
- Narrative information about medical, practical, and psychosocial issues.
This study addressed the relative appeal and value of these two components separately for White and African American women who had been diagnosed with breast cancer (three-fourths of participants had early-stage disease). The average time spent online with either type of resource was slightly longer for African American women (didactic: 19.7 minutes, standard deviation [SD] = 31.10; narrative: 17.16 minutes, SD = 38.19) than for White women (didactic: 18.30 minutes, SD = 28.62; narrative: 15.78 minutes, SD = 36.60) but had substantially more effect.
Before using the resource, African American women were markedly lower in health care participation; after use, African American women increased health care participation markedly, regardless of the type of resource, and surpassed the level of health care participation by White women, particularly in regard to the effect of the didactic services. This result suggests that while use of both the didactic and narrative CHESS resources is valuable for both groups, it is particularly useful for African American women; the narrative resource version appears to differentially have more impact for White women.
References:
- National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology: Distress Management. Version 2.2023. Plymouth Meeting, Pa: National Comprehensive Cancer Network, 2022.
Available online with free registration . Last accessed April 11, 2023. - Fashoyin-Aje LA, Martinez KA, Dy SM: New patient-centered care standards from the commission on cancer: opportunities and challenges. J Support Oncol 10 (3): 107-11, 2012 May-Jun.
- Andersen BL: Biobehavioral outcomes following psychological interventions for cancer patients. J Consult Clin Psychol 70 (3): 590-610, 2002.
- Meyer TJ, Mark MM: Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychol 14 (2): 101-8, 1995.
- Sheard T, Maguire P: The effect of psychological interventions on anxiety and depression in cancer patients: results of two meta-analyses. Br J Cancer 80 (11): 1770-80, 1999.
- Barsevick AM, Sweeney C, Haney E, et al.: A systematic qualitative analysis of psychoeducational interventions for depression in patients with cancer. Oncol Nurs Forum 29 (1): 73-84; quiz 85-7, 2002 Jan-Feb.
- Antoni MH, Lehman JM, Kilbourn KM, et al.: Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol 20 (1): 20-32, 2001.
- Budin WC, Hoskins CN, Haber J, et al.: Breast cancer: education, counseling, and adjustment among patients and partners: a randomized clinical trial. Nurs Res 57 (3): 199-213, 2008 May-Jun.
- Scheier MF, Helgeson VS, Schulz R, et al.: Interventions to enhance physical and psychological functioning among younger women who are ending nonhormonal adjuvant treatment for early-stage breast cancer. J Clin Oncol 23 (19): 4298-311, 2005.
- Antoni MH, Wimberly SR, Lechner SC, et al.: Reduction of cancer-specific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiatry 163 (10): 1791-7, 2006.
- Andersen BL, Farrar WB, Golden-Kreutz DM, et al.: Psychological, behavioral, and immune changes after a psychological intervention: a clinical trial. J Clin Oncol 22 (17): 3570-80, 2004.
- Jacobsen PB, Meade CD, Stein KD, et al.: Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J Clin Oncol 20 (12): 2851-62, 2002.
- McQuellon RP, Wells M, Hoffman S, et al.: Reducing distress in cancer patients with an orientation program. Psychooncology 7 (3): 207-17, 1998 May-Jun.
- Wise M, Han JY, Shaw B, et al.: Effects of using online narrative and didactic information on healthcare participation for breast cancer patients. Patient Educ Couns 70 (3): 348-56, 2008.
The Adjustment Disorders
The adjustment disorders are a diagnostic category of the fifth edition of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-5),[
Four of the most common subtypes are:
- With depressed mood.
- With anxiety.
- With anxiety and depressed mood.
- With mixed disturbance of emotions and conduct (for patients who may be showing behavioral signs of an adjustment disorder, such as missing appointments or new substance abuse).
Prevalence
Nearly every cancer patient experiences what could be considered an identifiable stressor, whether that is diagnosis, treatment, recurrence, or side effects. The patient's response to the identifiable stressor determines the presence of an adjustment disorder.
Adjustment disorders are the most commonly diagnosed mental health issue in the oncology setting. A meta-analysis examining 70 studies across 14 countries with more than 10,000 participants in oncology settings, including hematological oncology, found a prevalence rate of approximately 20% among ambulatory cancer patients in active treatment.[
Additional reviews more focused on North American populations [
Treatment
Although few studies specifically target cancer patients diagnosed exclusively with adjustment disorder, a number of studies have shown the benefits of psychosocial interventions with adult cancer patients (e.g., meta-analysis).[
Group counseling
Investigators tested the efficacy of a 10-week, 2-hours-per-week group cognitive-behavioral stress management intervention.[
- Progressive muscle relaxation.
- Cognitive restructuring.
- Interpersonal stressor conflict resolution.
- Social support.
The control condition consisted of a day-long seminar in which participants received a condensed psychoeducational version of the intervention, with significantly less interaction among group members. Among intervention participants, results showed a decrease in depression and an increase in benefit-finding (i.e., reporting that having breast cancer had made positive contributions to their lives) and optimism.
In a larger randomized study (N = 199) conducted by the same research group [
Another study examined an 18-week, 1.5-hours-per-week group intervention consisting of psychological strategies designed to do the following:[
- Reduce stress.
- Enhance mood.
- Alter health behaviors (diet, exercise, smoking).
- Enhance adherence to cancer treatments.
Outcome measures included:
- Emotional distress.
- Health behaviors.
- Immune responses.
A total of 227 women, all of whom had undergone surgery for regional breast cancer, were randomly assigned to either the intervention group or an assessment-only control group. Compared with the control group, the intervention group showed significantly less anxiety, improved ability to access social support, more healthy-lifestyle behaviors (with specific improvements noted in dietary and smoking behaviors), and an improvement in symptom levels and functional status.[
Mindfulness-based therapy
A randomized controlled trial of a 6-week mindfulness-based stress reduction intervention, compared with usual care, was conducted with 84 female survivors of breast cancer.[
- Psychological measures (fear of recurrence, recurrence concerns, state-trait anxiety, and depression).
- Quality of life (physical functioning, role limitations, and energy).
In a study examining the efficacy of mindfulness-based stress reduction in breast cancer survivors,[
- Psychological symptoms (anxiety, fear of recurrence overall, and fear of recurrence symptoms).
- Physical symptoms (fatigue severity and fatigue interference).
The survivors with the highest baseline stress experienced the greatest benefit.
In an 8-week study of mindfulness-based cognitive therapy for men with advanced prostate cancer,[
Hypnosis and relaxation
In one study, a group of women scheduled for excisional breast biopsy (N = 90) were randomly assigned either to a brief session (15 minutes) of hypnosis and guided relaxation delivered by trained clinical psychologists on the day of surgery, or to an attention-control empathic listening session of equal length. Presurgery distress was measured using visual analog scales and the short version of the Profile of Mood States. The hypnosis session markedly decreased anticipatory anxiety and increased relaxation that was measured just before the biopsy was performed, suggesting that hypnosis- and relaxation-naïve patients can benefit from brief treatment before stressful situations.[
Cognitive-behavioral therapy
Cognitive-behavioral therapy (CBT) has been widely studied. A CBT approach is based on the idea that mental, emotional, and even physical symptoms partly stem from thoughts, feelings, and behaviors, resulting in poor adaptation.[
CBT includes a variety of techniques, such as:
- Relaxation training.
- Problem solving.[
18 ][Level of evidence: I] - Cognitive restructuring.
- Coping self-statements.
Most studies have combined a variety of these approaches into a multicomponent treatment strategy designed to alleviate specific symptoms. CBT approaches tend to be relatively short-term, brief interventions, well-suited to the oncology setting.[
- Usual care.
- Professionally led stress management.
- Self-administered stress management.
The two intervention groups received stress management training that included the following before the start of chemotherapy:
- Abdominal breathing.
- Progressive muscle relaxation training with guided imagery.
- Coping self-statements.
The professionally led intervention group met with a mental health professional who taught them the stress management skills in one 60-minute session. The self-administered group received a packet of training materials that included:
- A 15-minute videotape of instructions.
- A 12-page booklet on coping with chemotherapy.
- A 35-minute audiotape of relaxation training instructions.
Results showed enhanced quality of life over usual care in the self-administered group only. The professionally led group did not show any improvement in quality of life when compared with usual care.
In a randomized clinical trial for the treatment of adjustment disorders, 57 patients with mixed cancer types were randomly assigned to receive either an 8-week, individual, problem-focused CBT intervention or an 8-week, individual, supportive counseling intervention.[
Individual therapy that uses CBT techniques to focus on developing problem-solving skills for use across multiple life stressors has been shown to be useful for cancer patients.[
- Formulating the nature of problems.
- Brainstorming alternative solutions.
- Systematically evaluating potential consequences of a solution while deciding on the optimal ones.
- Evaluating the eventual outcome after solution implementation.
Participants in the intervention showed greater problem-solving skills, less multidimensional distress, and greater quality of life compared with their control-group counterparts.
A meta-analysis of 45 studies investigating 62 treatment-control comparisons found significant beneficial effects in emotional adjustment for adult cancer patients who participated in psychosocial interventions.[
Another study found that a cognitive behavioral intervention to teach problem-solving was effective in promoting better self-management of cancer-related symptoms, especially for patients aged 60 years or younger.[
Increasingly, CBT studies for cancer include biobehavioral outcomes. A three-arm, randomized, controlled trial (N = 159) demonstrated that two individual sessions (60–90 minutes/session) of CBT-based stress management intervention, administered 1 to 2 weeks before radical prostatectomy for men with prostate cancer, had a positive impact on a number of immune system parameters (higher natural killer cell cytotoxicity and circulating proinflammatory cytokines).[
Can psychosocial interventions increase survival?
The intriguing question of whether participation in a psychosocial group intervention can result in increased survival has been investigated since 1989. The original study [
Attempts to replicate the supportive-expressive group therapy findings were made in Canada,[
Literature reviews, including three meta-analyses [
In summary, the preponderance of evidence indicates that despite evidence of improved quality of life, it seems unlikely that a psychosocial intervention has much chance of contributing independently to survival time. This evidence has led some experts to suggest that continued research into this question is no longer warranted.[
Pharmacotherapy
No studies have specifically targeted a population of cancer patients diagnosed exclusively with adjustment disorder, in which the primary intervention was some form of pharmacotherapy. Given the nature of the adjustment disorders, clinical experience suggests that, if available, an initial trial of short-term counseling or psychotherapy designed to alter or eliminate the identified stressor (and thus alleviate symptoms) should be tried before pharmacotherapy.[
As mentioned previously, sometimes the adjustment disorder may progress to a more-severe mental disorder (e.g., major depressive disorder) and thus warrant consideration of pharmacotherapy. In addition, when the patient does not benefit from short-term psychotherapy, adding an appropriate psychotropic medication for a brief period of time (e.g., 2–3 weeks for antianxiety medications, 12 months for antidepressants) may facilitate the psychotherapy, allowing the patient to better employ available coping strategies. The specific pattern of emotional or behavioral symptoms will determine which type of psychotropic medication to consider. For more information, see Depression.
Current Clinical Trials
Use our
References:
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association, 2013.
- Mitchell AJ, Chan M, Bhatti H, et al.: Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 12 (2): 160-74, 2011.
- Miovic M, Block S: Psychiatric disorders in advanced cancer. Cancer 110 (8): 1665-76, 2007.
- Morasso G: Screening adjustment disorders related to mastectomy and its treatment. New Trends in Experimental and Clinical Psychiatry 13 (1): 90-3, 1997.
- Meyer TJ, Mark MM: Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychol 14 (2): 101-8, 1995.
- Greer S, Moorey S, Baruch JD, et al.: Adjuvant psychological therapy for patients with cancer: a prospective randomised trial. BMJ 304 (6828): 675-80, 1992.
- Telch CF, Telch MJ: Group coping skills instruction and supportive group therapy for cancer patients: a comparison of strategies. J Consult Clin Psychol 54 (6): 802-8, 1986.
- Penedo FJ, Dahn JR, Molton I, et al.: Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer 100 (1): 192-200, 2004.
- Goodwin PJ, Leszcz M, Ennis M, et al.: The effect of group psychosocial support on survival in metastatic breast cancer. N Engl J Med 345 (24): 1719-26, 2001.
- Antoni MH, Lehman JM, Kilbourn KM, et al.: Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol 20 (1): 20-32, 2001.
- Antoni MH, Wimberly SR, Lechner SC, et al.: Reduction of cancer-specific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiatry 163 (10): 1791-7, 2006.
- Andersen BL, Farrar WB, Golden-Kreutz DM, et al.: Psychological, behavioral, and immune changes after a psychological intervention: a clinical trial. J Clin Oncol 22 (17): 3570-80, 2004.
- Lengacher CA, Johnson-Mallard V, Post-White J, et al.: Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology 18 (12): 1261-72, 2009.
- Lengacher CA, Reich RR, Paterson CL, et al.: Examination of Broad Symptom Improvement Resulting From Mindfulness-Based Stress Reduction in Breast Cancer Survivors: A Randomized Controlled Trial. J Clin Oncol 34 (24): 2827-34, 2016.
- Chambers SK, Occhipinti S, Foley E, et al.: Mindfulness-Based Cognitive Therapy in Advanced Prostate Cancer: A Randomized Controlled Trial. J Clin Oncol 35 (3): 291-297, 2017.
- Schnur JB, Bovbjerg DH, David D, et al.: Hypnosis decreases presurgical distress in excisional breast biopsy patients. Anesth Analg 106 (2): 440-4, table of contents, 2008.
- Jacobsen PB, Hann DM: Cognitive-behavioral interventions. In: Holland JC, Breitbart W, Jacobsen PB, et al., eds.: Psycho-oncology. Oxford University Press, 1998, pp 717-29.
- Allen SM, Shah AC, Nezu AM, et al.: A problem-solving approach to stress reduction among younger women with breast carcinoma: a randomized controlled trial. Cancer 94 (12): 3089-100, 2002.
- Jacobsen PB, Meade CD, Stein KD, et al.: Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J Clin Oncol 20 (12): 2851-62, 2002.
- Moorey S, Greer S, Bliss J, et al.: A comparison of adjuvant psychological therapy and supportive counselling in patients with cancer. Psychooncology 7 (3): 218-28, 1998 May-Jun.
- Nezu AM, Nezu CM, Felgoise SH, et al.: Project Genesis: assessing the efficacy of problem-solving therapy for distressed adult cancer patients. J Consult Clin Psychol 71 (6): 1036-48, 2003.
- Fawzy FI, Cousins N, Fawzy NW, et al.: A structured psychiatric intervention for cancer patients. I. Changes over time in methods of coping and affective disturbance. Arch Gen Psychiatry 47 (8): 720-5, 1990.
- Heiney SP, McWayne J, Hurley TG, et al.: Efficacy of therapeutic group by telephone for women with breast cancer. Cancer Nurs 26 (6): 439-47, 2003.
- Sherwood P, Given BA, Given CW, et al.: A cognitive behavioral intervention for symptom management in patients with advanced cancer. Oncol Nurs Forum 32 (6): 1190-8, 2005.
- Cohen L, Parker PA, Vence L, et al.: Presurgical stress management improves postoperative immune function in men with prostate cancer undergoing radical prostatectomy. Psychosom Med 73 (3): 218-25, 2011.
- Spiegel D, Bloom JR, Kraemer HC, et al.: Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet 2 (8668): 888-91, 1989.
- Fawzy FI, Fawzy NW, Hyun CS, et al.: Malignant melanoma. Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Arch Gen Psychiatry 50 (9): 681-9, 1993.
- Fox BH: A hypothesis about Spiegel et al.'s 1989 paper on Psychosocial intervention and breast cancer survival. Psychooncology 7 (5): 361-70, 1998 Sep-Oct.
- Goodwin PJ, Leszcz M, Quirt G, et al.: Lessons learned from enrollment in the BEST study--a multicenter, randomized trial of group psychosocial support in metastatic breast cancer. J Clin Epidemiol 53 (1): 47-55, 2000.
- Classen C, Butler LD, Koopman C, et al.: Supportive-expressive group therapy and distress in patients with metastatic breast cancer: a randomized clinical intervention trial. Arch Gen Psychiatry 58 (5): 494-501, 2001.
- Kissane DW, Love A, Hatton A, et al.: Effect of cognitive-existential group therapy on survival in early-stage breast cancer. J Clin Oncol 22 (21): 4255-60, 2004.
- Newell SA, Sanson-Fisher RW, Savolainen NJ: Systematic review of psychological therapies for cancer patients: overview and recommendations for future research. J Natl Cancer Inst 94 (8): 558-84, 2002.
- Chow E, Tsao MN, Harth T: Does psychosocial intervention improve survival in cancer? A meta-analysis. Palliat Med 18 (1): 25-31, 2004.
- Smedslund G, Ringdal GI: Meta-analysis of the effects of psychosocial interventions on survival time in cancer patients. J Psychosom Res 57 (2): 123-31; discussion 133-5, 2004.
- Edwards AG, Hailey S, Maxwell M: Psychological interventions for women with metastatic breast cancer. Cochrane Database Syst Rev (2): CD004253, 2004.
- Kissane DW: Survival following psychotherapy interventions. In: Holland JC, Breitbart WS, Jacobsen PB, et al., eds.: Psycho-oncology. 2nd ed. Oxford University Press, Inc., 2010, pp 479-82.
- Andersen BL, Yang HC, Farrar WB, et al.: Psychologic intervention improves survival for breast cancer patients: a randomized clinical trial. Cancer 113 (12): 3450-8, 2008.
- Coyne JC, Stefanek M, Palmer SC: Psychotherapy and survival in cancer: the conflict between hope and evidence. Psychol Bull 133 (3): 367-94, 2007.
- Strain JJ: Adjustment disorders. In: Holland JC, Breitbart W, Jacobsen PB, et al., eds.: Psycho-oncology. Oxford University Press, 1998, pp 509-17.
Anxiety Disorders: Description and Etiology
Anxiety occurs to varying degrees in patients with cancer and may increase as the disease progresses or as treatment becomes more aggressive.[
Anxiety reactions that are more prolonged or intense can no longer be classified as adjustment disorders. These disorders can negatively affect quality of life, can interfere with a cancer patient's ability to function socially and emotionally, and require intervention.[
Other specific anxiety disorders—such as generalized anxiety, phobia, or panic disorder—are not as common among cancer patients and usually predate the cancer diagnosis, but these disorders deserve further attention to facilitate cancer care. The stress caused by a diagnosis of cancer and its treatment may precipitate a relapse of preexisting anxiety disorders. These disorders can be disabling and can interfere with treatment. They require prompt diagnosis and effective management.[
Factors that can increase the likelihood of developing anxiety disorders during cancer treatment include the following:
- History of anxiety disorders.
- Severe pain or other physical symptoms (untreated anxiety disorders can also escalate the pain experience).[
7 ,8 ] - Anxiety at time of diagnosis.[
9 ] - Functional limitations.
- Lack of social support.[
2 ] - Advancing disease.
- History of trauma.[
1 ,10 ]
Some medical conditions and interventions are associated with symptoms that present as anxiety disorders, including:
- Central nervous system metastases.
- Dyspnea associated with lung cancer.
- Treatment with corticosteroids and other medications.
A patient's experience with cancer or other illnesses may reactivate associations and memories of previous illness and contribute to acute anxiety. Certain demographic factors, such as being female and developing cancer at a young age, are associated with increased anxiety in medical situations.[
Anxiety, on the other hand, can lead to overestimation of negative prognosis. A longitudinal study of women with ductal carcinoma in situ (N = 487) found that anxiety as measured by the Hospital Anxiety and Depression Scale was the factor that was most consistently and strongly associated with inaccurate perception of and overestimation of future breast cancer–related risks.[
In the patient with advanced disease, anxiety is often caused not by the fear of death but by the issues of uncontrolled pain, isolation, abandonment, and dependency.[
Anxiety Disorder Caused by Other General Medical Conditions
The following table highlights possible causes of anxiety in cancer patients.
| Medical Problem | Examples |
|---|---|
| a Adapted from Massie.[ |
|
| Poorly controlled pain | Insufficient or as-needed pain medications. |
| Abnormal metabolic states | Hypoxia, pulmonary embolus, sepsis, delirium, hypoglycemia, bleeding, coronary occlusion, or heart failure. |
| Hormone-secreting tumors | Pheochromocytoma, thyroid adenoma or carcinoma, parathyroid adenoma, corticotropin-producing tumors, and insulinoma. |
| Anxiety-producing drugs | Corticosteroids, neuroleptics used as antiemetics, thyroxine, bronchodilators, beta-adrenergic stimulants, antihistamines, and benzodiazepines (paradoxical reactions are often seen in older persons). |
| Anxiety-producing conditions | Substance withdrawal (from alcohol, opioids, or sedative-hypnotics). |
Patients in severe pain are anxious and agitated, and anxiety can potentiate pain. To adequately manage pain, the patient's anxiety must be treated.[
Acute onset of anxiety may be a precursor of a change in the metabolic state or of another impending medical event, such as myocardial infarction, infection, or pneumonia. Sepsis and electrolyte abnormalities can also cause anxiety symptoms. Sudden anxiety with chest pain or respiratory distress may suggest a pulmonary embolism. Patients who are hypoxic can experience anxiety; they may fear that they are suffocating.
Many drugs can precipitate anxiety in persons who are ill. For example, corticosteroids can produce motor restlessness, agitation, and mania as well as depression and thoughts of suicide. Bronchodilators and B-adrenergic receptor stimulants used for chronic respiratory conditions can cause anxiety, irritability, and tremulousness. Akathisia, or motor restlessness accompanied by subjective feelings of distress, is a side effect of neuroleptic drugs, which are commonly used for control of emesis. Withdrawal from opioids, benzodiazepines, barbiturates, nicotine, and alcohol can result in anxiety, agitation, and behaviors that may be problematic for the patient who is in active treatment.
Certain tumor sites can produce symptoms that resemble anxiety disorders. Pheochromocytomas and pituitary microadenomas can present as episodes of panic and anxiety.[
Primary Anxiety Disorders
Patients who have the following symptoms may be experiencing a specific anxiety disorder that was present before they became ill with cancer and that recurs because of the stress of the diagnosis and treatment:
- Intense fear.
- Inability to absorb information.
- Inability to cooperate with medical procedures.
Somatic symptoms include the following:
- Shortness of breath.
- Sweating.
- Lightheadedness.
- Palpitations.
Patients with cancer can present with any of multiple anxiety disorders diagnosed via the criteria of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), including:
- Phobias.
- Panic disorder.
- Generalized anxiety disorder.
- Obsessive-compulsive disorder (potentially in the form of obsessiveness about cancer recurrence).
- Health anxiety disorder.
- Post-traumatic stress disorder (if related to cancer diagnosis; see Cancer-Related Post-Traumatic Stress for more information).
- Anxiety disorder that is caused by another medical condition.
Patients with these anxiety disorders are generally distressed about their symptoms and are usually compliant with behavioral and psychopharmacological intervention.[
Phobias
Phobias are persistent fears or avoidance of a circumscribed object or situation. People with phobias usually experience intense anxiety and avoid potentially frightening situations. Phobias are experienced by cancer patients in a number of ways, such as fear of witnessing blood or tissue injury (also known as needle phobia) or claustrophobia (for example, during a magnetic resonance imaging scan). Phobias can complicate medical procedures and can result in the refusal of necessary medical intervention or tests.[
Panic disorder
In panic disorder, intense, rapid-onset anxiety is the predominant symptom, virtually always accompanied by severe somatic symptoms that may include the following:
- Shortness of breath.
- Dizziness.
- Palpitations.
- Nausea.
- Fears of going crazy or that a heart attack is occurring.
Panic disorder is characterized by discrete panic attacks that are experienced as happening suddenly, often without a specific trigger, and become intense very quickly. Attacks are self-limiting and generally last for 10 to 20 minutes, though the psychological discomfort and fear of recurrence may last longer. Patients with panic attacks often present with symptoms that can be difficult to differentiate from other medical disorders, though a known history of panic disorder can help clarify the diagnosis. Panic disorder in patients with cancer is most often managed with benzodiazepines and antidepressant medications [
Generalized anxiety disorder
Generalized anxiety disorder is characterized by ongoing, unrealistic, and excessive anxiety and worry about two or more life circumstances, to a degree that is pervasive and does not respond to either reassurance or contrary evidence. The following physical symptoms may be reported but do not have the sudden onset or intensity of panic attacks:
- Motor tension (restlessness, muscle tension, and being easily fatigued).
- Autonomic hyperactivity (shortness of breath, heart palpitations, sweating, and dizziness).
- Vigilance in scanning (feeling keyed up and on edge, irritability, and having exaggerated startle responses).
Obsessive-compulsive disorder
Obsessive-compulsive disorder (OCD) is characterized by persistent thoughts, ideas, or images (obsessions) and by repetitive, purposeful, and intentional behaviors (compulsions) that a person performs to manage his or her intense distress. To qualify as OCD, the obsessive thoughts and compulsive behaviors must be time-consuming and sufficiently distracting to interfere with the person's ability to function in employment, academic, or social situations.
Patients with cancer who have a history of OCD may engage in compulsive behaviors such as hand washing, checking, or counting to such an extent that they cannot comply with treatment. For such patients, normal worry about the cancer diagnosis and prognosis can develop into full obsessive-compulsive symptoms and be severely disabling. OCD is most often managed with serotonergic antidepressant medications (selective serotonin reuptake inhibitors [SSRIs] and clomipramine) and CBT. Milder obsessive thoughts or use of rituals that are not interfering might be addressed with CBT, but medications are not indicated. This disorder is rare in cancer patients who do not have a premorbid history of some type of anxiety disorder.
Health anxiety disorder
Cancer survivors have been known to develop health anxiety disorder related to their fears of recurrence, including:[
- Hypervigilance to potential physical symptoms.
- Somatization.
- Extreme focus on cancer status.
- Identification with the patient role in care settings.
- Requesting frequent care, even after high-maintenance care needs have ended (including, but not limited to, requests for additional office visits and premature maintenance scans).
Although research is still ongoing, early clinical guidelines suggest that CBT and treatment with SSRIs may be beneficial.
A study conducted in posttreatment cancer-free survivors (N = 133) investigated the full spectrum of anxiety disorders using standardized diagnostic and dimensional assessments.[
- Generalized anxiety disorder (41%).
- Specific phobias (14%).
- Social anxiety disorder (13%).
A large number of survivors reporting generalized anxiety (74%) and social anxiety (62%) had onset of symptoms after cancer diagnosis and associated their symptoms with cancer. Generalized anxiety was often triggered by cancer-related changes in perceived health and vulnerability, and social anxiety was associated with cancer-related changes in appearance, self-perceptions, and lack of social connectedness. In survivors with no history of anxiety disorders, lingering treatment-related side effects predicted the onset of the first anxiety disorder episode. In survivors with a history of anxiety disorders, a higher cancer stage predicted development of anxiety disorder symptoms.[
Screening and Assessment
Effective management of anxiety disorders begins with a thorough and comprehensive assessment and an accurate diagnosis. The normal fears and uncertainties associated with cancer are often intense. Frequently not clear is the distinction between normal fears and fears that are more severe and reach the criteria for an anxiety disorder. For more information, see Table 3 .[
Treatment considerations should take into account the patient's quality of life and not be based solely on the disorder. To assess the severity of the anxiety, it is important to understand how much the symptoms of anxiety interfere with activities of daily living. Screening for anxiety could include a brief self-report questionnaire that, if a defined cutoff score is exceeded, could then be followed by a more-thorough clinical interview. A variety of general screening questionnaires have been used to identify distress. Other anxiety-specific self-report questionnaires (e.g., State-Trait Anxiety Inventory) have also been used, and a questionnaire for the assessment of prostate cancer–related anxiety has been developed and validated.[
The following is a list of symptoms designed to distinguish common or normal worry from more-serious symptoms of anxiety. When patients report the more-serious symptoms, referral to a qualified mental health professional may be warranted.
| Symptoms of Common or Normal Worry | More-Serious Symptoms of Anxiety Disorders |
|---|---|
| a Adapted from Nicholas.[ |
|
| Worry comes and goes. | Worry seems constant. |
| Has some difficulty in concentrating. | Is unable to concentrate. |
| Is able to "turn off thoughts" most of the time. | Is unable to "turn off thoughts" most of the time. |
| Has occasional trouble falling asleep. | Has trouble falling asleep and/or wakes up early most nights. |
| Has occasional crying spells that seem to provide some relief. | Has frequent crying spells that interfere with daily activities. |
| Fear and apprehension are clearly connected to some upcoming event (e.g., start of treatment, doctor's appointment, or receipt of test results). | Fear and apprehension are more "free floating" and seem to be present most of the time. |
| Has few, if any, physical symptoms (e.g., racing heart, dry mouth, shaky hands, or restlessness). | Has many physical symptoms (e.g., racing heart, dry mouth, shaky hands, restlessness, fidgetiness, or feeling keyed up). |
| Has ways to reduce anxiety (e.g., distraction by staying busy). | Has few, if any, ways to reduce anxiety. |
Interventions
When anxiety is situational (i.e., produced by pain, another underlying medical condition, a hormone-secreting tumor, or a side effect of medication), the prompt treatment of the cause usually leads to immediate control of the symptoms.[
Initial management of anxiety includes providing adequate information and support to the patient. Initial symptoms, which may warrant a psychiatric or psychological consultation, may first be reported to the primary oncologist or surgeon.[
Psychosocial interventions
Psychological approaches include:[
- Combinations of CBT techniques.
- Insight-oriented psychotherapy.
- Crisis intervention.
- Couple and family therapy.
- Group therapy.
- Self-help groups.
- Relaxation-based interventions.
Hypnosis, meditation, progressive relaxation, guided imagery, and biofeedback can be used to treat anxiety symptoms that are associated with the following:
- Painful procedures.
- Pain syndromes.
- Crisis situations.
- Anticipatory fears.
- Depressive syndromes.
Combining different approaches can be beneficial for some patients. Referring patients who may be struggling with anxiety disorders for full assessment and psychological treatment will enhance participation in care, improve quality of life, and reduce the pain experience.[
One study of 509 recurrence-free breast cancer survivors at 5 to 9 years posttreatment examined the usefulness of a comprehensive intervention that combined positive coping strategies based on CBT (e.g., calming self-talk or relaxation) with education about the disease, treatment, and potential side effects.[
Preliminary evidence suggests racial differences in the use and benefit of specific coping strategies (e.g., religious coping strategies, such as prayer and hopefulness, are used more by African American women and provide greater benefit for these women).[
Pharmacological interventions
Patients with cancer often have symptoms of both anxiety and depression caused by stressors related to cancer treatment. Such symptoms of distress often are resolved with psychological support alone; however, in some cases, pharmacological interventions are required. For descriptions of symptoms of anxiety disorders possibly requiring pharmacological treatment, see Table 3.
Following are brief descriptions of pharmacological treatment options and potential indications for their use. These descriptions are based on evidence derived from studies conducted in patients without cancer because of the lack of such studies in patients with cancer. However, clinicians have used some of these medications for several decades to treat anxiety symptoms in patients with cancer. The treatment options and their use in the situations described below are also based on clinical experience with these agents in patients with cancer.
The use of medications to treat anxiety disorders is considered when patients experience more-severe symptoms or when their responses to psychosocial interventions are inadequate. When counseling resources are not available or the patient declines them, medication may be considered sooner rather than later. In certain cases, medications are started simultaneously with psychosocial interventions when it is likely that psychosocial support alone will be inadequate to provide relief or to provide it soon enough.
Pharmacological interventions can be used short-term or long-term, depending on individual patient and illness factors, including the following:
- Severity of anxiety symptoms.
- Level of functional/social impairment.
- Psychiatric history.
- Continued presence of cancer.
- Cancer treatment–related factors contributing to anxiety directly or indirectly (e.g., high-intensity or long-term cancer treatments or treatment with agents known to cause to psychiatric symptoms [e.g., cytokines]).
Specific anxiety medications—i.e., medications from the benzodiazepine class, as listed in Table 4 —are frequently used alone or in combination with psychological approaches to provide relief from anxiety symptoms. These medications are effective in the acute treatment of anxiety disorders because of their rapid onset of action. They are frequently used as monotherapy or as adjunctive agents in the short-term management (<4 months) of anxiety disorders. Their long-term use (>4 months) is limited by the potential for abuse and dependence and by their lack of antidepressant effects, as depression is often comorbid with anxiety disorders. Following are some of the indications and safety considerations for the use of benzodiazepines in patients with cancer:[
- Short-acting benzodiazepines, such as alprazolam and lorazepam, can be effectively used to provide short-term relief at specific points in the cancer continuum of diagnosis, treatment, and recurrence. Examples of such short-term use include the treatment of anxiety during diagnostic procedures (e.g., certain radioimaging procedures) and about pending test results (e.g., for yearly mammograms in patients with a history of breast cancer).
- Cancer treatments, such as intensive chemotherapeutic regimens, can cause significant physical and emotional distress and exacerbate anxiety. Short-acting or intermediate-acting agents (e.g., clonazepam) can provide significant relief of anxiety and other symptoms (e.g., insomnia secondary to anxiety) during active cancer treatments.
- Longer-acting medications (e.g., diazepam and clorazepate) should generally be avoided because of their long half-lives. These medications can cause or exacerbate cognitive impairment, disorientation, and drowsiness because of their potential for accumulation.
- Patients with medical conditions such as delirium can present with anxiety and agitation. Benzodiazepine use in patients with such conditions is contraindicated because these agents can cause or exacerbate confusion and disorientation.
- All patients, especially elderly patients, receiving benzodiazepines should be closely monitored for cognitive impairment, daytime sedation, and fall risks. Use of these agents should be optimized in elderly patients, patients with multiple comorbidities, patients with liver disease, and patients receiving multiple medications.
- Use of these agents should be closely monitored and optimized in patients receiving other sedating medications, central nervous system depressants, and agents with potential for causing respiratory depression (e.g., opiates).
- It is important to continuously monitor and reevaluate anxiety symptoms in all patients receiving benzodiazepines. Use of these medications can be tapered off if anxiety symptoms resolve after cancer treatment ends.
- In some patients, the use of benzodiazepines is continued (as monotherapy or adjunctive treatment) over a longer period (>4 months) because of persistent and debilitating anxiety symptoms. It is important to monitor the development of tolerance, abuse, and dependence issues as well as comorbid depressive symptoms in such patients. Long-term and sometimes chronic use of these agents might be indicated in a subpopulation of patients, with close monitoring and frequent risk-benefit assessments. Persistent (after 3 or 4 months) anxiety symptoms frequently lead to depression. Patients with persistent anxiety symptoms with or without depression might benefit from alternative treatments (e.g., paroxetine, sertraline).
| bid = twice a day; CYP = cytochrome P450 enzyme; qd = once a day; qid = 4 times a day; tid = 3 times a day. | |||
| a Adapted from Lorenz et al.,[ |
|||
| b For dosing information for antidepressants used to treat anxiety, see Depression. | |||
| Benzodiazepines | • Use acutely, then taper off as tolerated. | ||
| Drugb | Starting Dose (Range) | Comment(s) | Reference(s) |
| Alprazolam | 0.25–0.5 mg tid (≤4 mg/d) | Available in sustained-release form. | [ |
| Chlordiazepoxide | 5–10 mg tid–qid | No maximum dose listed. | [ |
| Titrate carefully >40 mg/d. | |||
| Clonazepam | 0.125–0.25 mg bid–tid (≤4 mg/d) | More commonly used. | [ |
| Clorazepate | 30 mg/d in 2–3 doses (≤60 mg/d) | [ |
|
| Diazepam | 2–10 mg bid–qid | No maximum dose listed. | [ |
| Titrate carefully >40 mg/d. | |||
| Lorazepam | 0.5–1 mg bid–tid (≤10 mg/d) | Preferred in liver disease. | [ |
| More commonly used. | |||
| Oxazepam | 10–15 mg tid–qid | No maximum dose listed. | [ |
| Titrate carefully >120 mg/d. | |||
| Preferred in liver disease. | |||
| Antidepressants | • Use if long-term therapy is needed. | ||
| • Use with caution with tamoxifen because of CYP2D6 interactions. | |||
| Drugb | Starting Dose (Range) | Comment(s) | Reference |
| Citalopram | 10–40 mg/d | QTc prolongation. | [ |
| Preferred with tamoxifen. | |||
| Desipramine | 25–200 mg/d | Use with caution in elderly patients. | [ |
| Duloxetine | 20–60 mg/d | [ |
|
| Escitalopram | 5–20 mg/d | QTc prolongation. | [ |
| Preferred with tamoxifen. | |||
| Fluoxetine | 10–60 mg/d | Do not use with tamoxifen. | [ |
| Imipramine | 10–200 mg/d | Use with caution in elderly patients. | [ |
| Mirtazapine | 7.5–45 mg/d | [ |
|
| Paroxetine | 10–40 mg/d | Do not use with tamoxifen. | [ |
| Sertraline | 25–200 mg/d | [ |
|
| Venlafaxine | 37.5–225 mg/d | [ |
|
| Other Drugs | |||
| Drugb | Starting Dose (Range) | Comment(s) | Reference |
| Buspirone | 7.5 mg bid | ≤30 mg/d for anxiety. | [ |
| Hydroxyzine | 50–100 mg qid | [ |
|
| Antipsychotics | • Consider for treatment-refractory anxiety. | ||
| • Most associated with significant weight gain. | |||
| • Also evaluate for metabolic syndrome, cardiovascular and cerebrovascular side effects. | |||
| • Risk of QTc prolongation and extrapyramidal side effects. | |||
| Drugb | Starting Dose (Range) | Comment(s) | Reference |
| Aripiprazole | 2–10 mg/d | Titrate carefully >15 mg/d. | [ |
| Haloperidol | 0.5–2 mg bid–tid | [ |
|
| Olanzapine | 2.5–10 mg/d | [ |
|
| Quetiapine | 12.5–25 mg/d | May titrate >300 mg/d. | [ |
| Benefit seen in some trials. | |||
| Risperidone | 0.5–1 mg qd–bid | Titrate carefully >2 mg/d. | [ |
The choice of a benzodiazepine depends on the following:
- Duration of action that is best suited to the patient.
- Desired rapidity of onset needed.
- Route of administration available.
- Presence or absence of active metabolites.
- Metabolic problems.
Dosing schedules depend on patient tolerance and require individual titration. The shorter-acting benzodiazepines (alprazolam and lorazepam) are given 3 to 4 times per day. Short-acting benzodiazepines, particularly those that can be administered by multiple routes (lorazepam and diazepam), are effective for high levels of distress. Benzodiazepines decrease daytime anxiety and reduce insomnia. The most common side effects of benzodiazepines are dose dependent and are controlled by titrating the dose to avoid drowsiness, confusion, motor incoordination, and sedation. For more information, see Sleep Disorders.
All benzodiazepines can cause some degree of respiratory depression, which is generally minimal in patients who have not used benzodiazepines in the past. Benzodiazepines should be used cautiously (or not at all) in cases of respiratory impairment.
Standard precautions should be considered when any sedative is used in patients who have borderline respiratory function. Ongoing assessment of this population is important. Low doses of the antihistamine hydroxyzine (25 mg, 2–3 times a day) can be used safely in such situations. In patients with hepatic dysfunction, it is best to use short-acting benzodiazepines that are metabolized primarily by conjugation and excreted by the kidneys (e.g., oxazepam, temazepam, or lorazepam). Another advantage of using lorazepam is its lack of active metabolites. Conversely, other benzodiazepines should be selected in cases of renal dysfunction.
SSRIs (e.g., fluoxetine and sertraline) and serotonin-norepinephrine reuptake inhibitors (SNRIs) (e.g., venlafaxine) are considered first-line pharmacotherapy for long-term management of anxiety disorders. SSRIs and SNRIs are also effective in the treatment of depressive symptoms frequently comorbid with persistent anxiety disorders. SSRIs and SNRIs can take approximately 4 to 6 weeks to take effect because of their slow onset of action. Benzodiazepines are frequently used as adjunctive agents to stabilize symptoms in the initial period of treatment with SSRIs and SNRIs.
Atypical antidepressants (e.g., mirtazapine) are sometimes used to treat anxiety disorders because of their added effects on comorbid symptoms, such as insomnia. Older medications, such as tricyclic antidepressants (e.g., imipramine and clomipramine) and monoamine oxidase inhibitors (e.g., phenelzine), are also effective in treating anxiety disorders. The use of antidepressants in clinical practice is limited by their unfavorable side effects, poorer tolerability, and higher risks of toxicity.[
For more information, see the Suicide Risk in Cancer Patients section in Depression.
Buspirone, a nonbenzodiazepine, is useful in patients who have not previously been treated with a benzodiazepine and in those who may abuse benzodiazepines (e.g., those with a history of illicit substance abuse or alcoholism). Buspirone is also useful in the geriatric population to augment fluoxetine for the treatment of anxiety and depression. The beginning dose is 5 mg 3 times a day and can be increased to 15 mg 3 times a day. Buspirone can also be given twice a day.
The use of specific classes of medications is considered for managing treatment-refractory anxiety symptoms or in certain clinical situations. Low-dose neuroleptics (e.g., thioridazine, 10 mg 3 times a day; and risperidone, 1 mg twice a day) are used to treat severe anxiety when an adequate dose of a benzodiazepine is ineffective or if the patient might be expected to respond poorly to benzodiazepines (e.g., patients with brain metastases). Low-dose neuroleptics can also be used when benzodiazepines are not helpful or when there is the possibility of delirium, dementia, or other complications. Low-dose anticonvulsants (e.g., pregabalin, 200 mg per day) are sometimes used to treat severe treatment-resistant anxiety when other medications are ineffective or contraindicated because of certain associated risks.[
The presence or absence of specific psychiatric or medical comorbidities is frequently a critical factor in the selection of pharmacological treatments. Pharmacokinetic and pharmacodynamic interactions with other medications are also important factors to consider in the selection of agents. Following are some examples of such factors and clinical situations driving the selection of pharmacological treatments:
- When depressive symptoms are comorbid with anxiety, treatment with SSRIs, SNRIs, or other antidepressants is strongly considered.
- When neuropathic pain is comorbid with anxiety symptoms, specific antidepressants with known efficacy in treating neuropathic pain (e.g., duloxetine and venlafaxine) are considered.
- When hot flashes are comorbid with anxiety symptoms, specific agents with known efficacy in treating hot flashes (e.g., venlafaxine) are considered.
- Specific medications with known side effects (e.g., nausea with duloxetine or risk of sedation with mirtazapine) are avoided when patients are already experiencing these side effects from their cancer treatments and because of the possible exacerbation of these side effects.
- Patients who are treated with CYP2D6 inhibitors (e.g., paroxetine) and tamoxifen may be at risk of significant drug-drug interactions. For more information, see Hot Flashes and Night Sweats.
No pharmacological treatment studies have been conducted in children and adolescents with cancer. Furthermore, evidence for pharmacological treatment of anxiety disorders in pediatric patients without cancer is also limited. One meta-analysis of pediatric antidepressant clinical trials [
In general, patients with cancer need to be encouraged to take enough medication to relieve anxiety. Medications are readily tapered and discontinued when symptoms subside. Concerns about addiction are exaggerated in patients with cancer and often interfere with adequate symptom relief.
Current Clinical Trials
Use our
References:
- Breitbart W: Identifying patients at risk for, and treatment of major psychiatric complications of cancer. Support Care Cancer 3 (1): 45-60, 1995.
- Stark D, Kiely M, Smith A, et al.: Anxiety disorders in cancer patients: their nature, associations, and relation to quality of life. J Clin Oncol 20 (14): 3137-48, 2002.
- Schag CA, Heinrich RL: Anxiety in medical situations: adult cancer patients. J Clin Psychol 45 (1): 20-7, 1989.
- Mitchell AJ, Chan M, Bhatti H, et al.: Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 12 (2): 160-74, 2011.
- Razavi D, Stiefel F: Common psychiatric disorders in cancer patients. I. Adjustment disorders and depressive disorders. Support Care Cancer 2 (4): 223-32, 1994.
- Maguire P, Faulkner A, Regnard C: Managing the anxious patient with advancing disease--a flow diagram. Palliat Med 7 (3): 239-44, 1993.
- Fischer DJ, Villines D, Kim YO, et al.: Anxiety, depression, and pain: differences by primary cancer. Support Care Cancer 18 (7): 801-10, 2010.
- Suskin JA, Paul S, Stuckey AR, et al.: Risk factors for worse anxiety trajectories among patients undergoing cancer chemotherapy. Support Care Cancer 31 (1): 32, 2022.
- Nordin K, Glimelius B: Predicting delayed anxiety and depression in patients with gastrointestinal cancer. Br J Cancer 79 (3-4): 525-9, 1999.
- Green BL, Krupnick JL, Rowland JH, et al.: Trauma history as a predictor of psychologic symptoms in women with breast cancer. J Clin Oncol 18 (5): 1084-93, 2000.
- Friedman LC, Lehane D, Webb JA, et al.: Anxiety in medical situations and chemotherapy-related problems among cancer patients. J Cancer Educ 9 (1): 37-41, 1994.
- Partridge A, Adloff K, Blood E, et al.: Risk perceptions and psychosocial outcomes of women with ductal carcinoma in situ: longitudinal results from a cohort study. J Natl Cancer Inst 100 (4): 243-51, 2008.
- Hackett TP, Cassem NH: Massachusetts General Hospital Handbook of General Hospital Psychiatry. 2nd ed. PSG, 1987.
- Massie MJ: Anxiety, panic, and phobias. In: Holland JC, Rowland JH, eds.: Handbook of Psychooncology: Psychological Care of the Patient With Cancer. Oxford University Press, 1989, pp 300-9.
- Velikova G, Selby PJ, Snaith PR, et al.: The relationship of cancer pain to anxiety. Psychother Psychosom 63 (3-4): 181-4, 1995.
- Glover J, Dibble SL, Dodd MJ, et al.: Mood states of oncology outpatients: does pain make a difference? J Pain Symptom Manage 10 (2): 120-8, 1995.
- Wilcox JA: Pituitary microadenoma presenting as panic attacks. Br J Psychiatry 158: 426-7, 1991.
- Stark DP, House A: Anxiety in cancer patients. Br J Cancer 83 (10): 1261-7, 2000.
- Arch JJ, Genung SR, Ferris MC, et al.: Presence and predictors of anxiety disorder onset following cancer diagnosis among anxious cancer survivors. Support Care Cancer 28 (9): 4425-4433, 2020.
- Roth AJ, Rosenfeld B, Kornblith AB, et al.: The memorial anxiety scale for prostate cancer: validation of a new scale to measure anxiety in men with prostate cancer. Cancer 97 (11): 2910-8, 2003.
- Roth A, Nelson CJ, Rosenfeld B, et al.: Assessing anxiety in men with prostate cancer: further data on the reliability and validity of the Memorial Anxiety Scale for Prostate Cancer (MAX-PC). Psychosomatics 47 (4): 340-7, 2006 Jul-Aug.
- Nicholas DR: Emotional Side Effects of Cancer: Distinguishing Normal Distress from Mental Disorders [brochure]. Ball Memorial Hospital and Ball State University, 2008.
- Hinshaw DB, Carnahan JM, Johnson DL: Depression, anxiety, and asthenia in advanced illness. J Am Coll Surg 195 (2): 271-7; discussion 277-8, 2002.
- Montazeri A, Jarvandi S, Haghighat S, et al.: Anxiety and depression in breast cancer patients before and after participation in a cancer support group. Patient Educ Couns 45 (3): 195-8, 2001.
- Brown LF, Kroenke K, Theobald DE, et al.: The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Psychooncology 19 (7): 734-41, 2010.
- Osborn RL, Demoncada AC, Feuerstein M: Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med 36 (1): 13-34, 2006.
- Gil KM, Mishel MH, Germino B, et al.: Uncertainty management intervention for older African American and Caucasian long-term breast cancer survivors. J Psychosoc Oncol 23 (2-3): 3-21, 2005.
- Reddick BK, Nanda JP, Campbell L, et al.: Examining the influence of coping with pain on depression, anxiety, and fatigue among women with breast cancer. J Psychosoc Oncol 23 (2-3): 137-57, 2005.
- Stiefel F, Berney A, Mazzocato C: Psychopharmacology in supportive care in cancer: a review for the clinician. I. Benzodiazepines. Support Care Cancer 7 (6): 379-85, 1999.
- Michael Kaplan E, DuPont RL: Benzodiazepines and anxiety disorders: a review for the practicing physician. Curr Med Res Opin 21 (6): 941-50, 2005.
- Lorenz RA, Jackson CW, Saitz M: Adjunctive use of atypical antipsychotics for treatment-resistant generalized anxiety disorder. Pharmacotherapy 30 (9): 942-51, 2010.
- Traeger L, Greer JA, Fernandez-Robles C, et al.: Evidence-based treatment of anxiety in patients with cancer. J Clin Oncol 30 (11): 1197-205, 2012.
- Lexicomp Online. Hudson, Ohio: Lexi-Comp, Inc., 2021.
Available online with subscription . Last accessed Feb. 9, 2024. - Hoffman EJ, Mathew SJ: Anxiety disorders: a comprehensive review of pharmacotherapies. Mt Sinai J Med 75 (3): 248-62, 2008 May-Jun.
- Bridge JA, Iyengar S, Salary CB, et al.: Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA 297 (15): 1683-96, 2007.
Considerations for Pediatric Patients and Their Families
Psychological Adjustment
Treatment of childhood cancer is a highly stressful experience, challenging and disruptive to children and their family members. It is therefore assumed that children undergoing cancer treatment are at significantly higher risk for depression, anxiety, and other indicators of psychological distress. However, the empirical evidence to support this assumption is weak. Overall, studies suggest that children treated for cancer and children who are long-term survivors of cancer experience few significant psychological adjustment problems.[
There is evidence that children experience distress during cancer treatment. Distress appears to be most significant early in therapy, typically when frequent hospitalizations are necessary, with a pattern of less distress occurring over time.[
The validity of obtaining accurate reports of psychological distress in this population has been questioned. One investigation examined whether psychological defensiveness might mask the reporting of depression and other symptoms of psychological distress. Researchers studied 107 children treated for cancer and 422 healthy controls, who completed a series of measures of depression and anxiety.[
Studies have reported no differences from controls on the following measures:
- Self-esteem.[
9 ,10 ] - Hopefulness.[
9 ] - Depression, anxiety, or loneliness.[
10 ]
One group of investigators [
Differences in Adjustment
Diagnosis and type of treatment appear to make a difference in adjustment in specific subgroups of children with cancer.[
Solid tumors
Children treated for solid tumors not involving the central nervous system (CNS) appear to have minimal psychological distress, and this is maintained after treatment.[
Acute lymphoblastic leukemia or lymphoma
Children treated for acute lymphoblastic leukemia or lymphoma report poorer emotional functioning, cognitive skills, autonomy, and family interaction than do children treated for non-CNS solid tumors.[
CNS tumors
For children whose disease or treatment directly involves the CNS, the risk of developing social and emotional problems appears much greater. Children with brain tumors are seen by their peers as being sick, fatigued, absent from school, and socially isolated and are less likely to be viewed as friends by their peers.[
Stem cell transplantation
Children receiving hematopoietic stem cell transplantation (HSCT) are likely to experience declines in both social competence and self-concept over time.[
Ethnicity
Ethnicity can also play a role in quality of life.[
Family factors
Family factors appear to play a large role in child adjustment, with family cohesion and expressiveness associated with better outcomes and family conflict associated with poorer outcomes, particularly for children experiencing more-intensive treatment.[
Siblings
The challenges of dealing with the diagnosis and treatment of childhood cancer also has implications for the coping and adjustment of siblings. During treatment, siblings of children with cancer may report:
- Higher levels of anxiety and loneliness than siblings of healthy children.[
20 ][Level of evidence: II] - Post-traumatic distress symptoms (reported by approximately 50% of siblings).[
21 ][Level of evidence: II] - Distress about family disruptions and separations.[
21 ] - Lack of attention associated with the focus of other family members on the ill child.[
21 ] - Negative interactions with family members.[
21 ] - Fear of the sibling's death.[
21 ]
Siblings of children with cancer also report becoming more compassionate and perceiving that their families are drawn closer together through the experience.[
The risk to families increases with the following conditions:
- Younger patient age.[
22 ] - Longer duration of cancer treatment.[
20 ] - Whether the child with cancer dies.[
23 ]
For siblings of children who undergo allogeneic HSCT, the risk for anxiety and lower self-esteem is higher for siblings who serve as hematopoietic stem cell donors, while nondonors are at higher risk of developing school problems.[
Childhood Cancer Survivor Study
The Childhood Cancer Survivor Study (CCSS) is a large, ongoing, multicenter study of more than 10,000 long-term survivors of childhood cancer and a comparison sibling control population. Using extensive survey methodology that links reports of current functioning to diagnosis, types of treatment, and other health factors associated with cancer and its treatment, the CCSS has selectively looked at long-term adjustment in large samples of young adults treated for similar childhood cancers. In one CCSS report, 2,778 survivors of solid tumors diagnosed in childhood and 2,925 siblings were surveyed using a standardized, long-term, follow-up questionnaire. Symptoms associated with depression, somatization, and anxiety were reported, along with demographic, health, and medical information. Cancer survivors reported few, if any, symptoms of psychological distress, although survivors of solid-tumor cancers reported higher levels of global distress than did their siblings. There were no differences on these measures from population norms. For both cancer survivors and their siblings, female gender, lower education and income attainment, perceived poor health status, and reports of current health problems were all associated with higher levels of psychological distress symptoms.[
The CCSS also reported positive findings for young adults who are survivors of leukemias and lymphomas. Follow-up questionnaires about psychological adjustment were administered to 5,736 young adult survivors of leukemia, non-Hodgkin lymphoma, and Hodgkin disease and to 2,565 adult siblings. Survivors reported higher levels of depressive symptoms and somatic distress than siblings, but neither group's scores fell within the clinically significant range for the general population. Sociodemographic factors such as gender and socioeconomic status were associated with reports of depressive symptoms, regardless of treatment status. The only disease-related factor associated with psychological distress was intensive chemotherapy, which was linked to an increase in somatic complaints.[
References:
- Eiser C, Hill JJ, Vance YH: Examining the psychological consequences of surviving childhood cancer: systematic review as a research method in pediatric psychology. J Pediatr Psychol 25 (6): 449-60, 2000.
- Zebrack BJ, Zeltzer LK, Whitton J, et al.: Psychological outcomes in long-term survivors of childhood leukemia, Hodgkin's disease, and non-Hodgkin's lymphoma: a report from the Childhood Cancer Survivor Study. Pediatrics 110 (1 Pt 1): 42-52, 2002.
- Zebrack BJ, Gurney JG, Oeffinger K, et al.: Psychological outcomes in long-term survivors of childhood brain cancer: a report from the childhood cancer survivor study. J Clin Oncol 22 (6): 999-1006, 2004.
- Sawyer M, Antoniou G, Toogood I, et al.: Childhood cancer: a 4-year prospective study of the psychological adjustment of children and parents. J Pediatr Hematol Oncol 22 (3): 214-20, 2000 May-Jun.
- Varni JW, Katz E: Stress, social support and negative affectivity in children with newly diagnosed cancer: a prospective transactional analysis. Psychooncology 6 (4): 267-78, 1997.
- Chao CC, Chen SH, Wang CY, et al.: Psychosocial adjustment among pediatric cancer patients and their parents. Psychiatry Clin Neurosci 57 (1): 75-81, 2003.
- Phipps S, Srivastava DK: Approaches to the measurement of depressive symptomatology in children with cancer: attempting to circumvent the effects of defensiveness. J Dev Behav Pediatr 20 (3): 150-6, 1999.
- Grootenhuis MA, Last BF, van der Wel M, et al.: Parents' attribution of positive characteristics to their children with cancer. Psychol Health 13: 67-81, 1998.
- Ritchie MA: Self-esteem and hopefulness in adolescents with cancer. J Pediatr Nurs 16 (1): 35-42, 2001.
- Noll RB, Gartstein MA, Vannatta K, et al.: Social, emotional, and behavioral functioning of children with cancer. Pediatrics 103 (1): 71-8, 1999.
- Levi RB, Drotar D: Health-related quality of life in childhood cancer: discrepancy in parent-child reports. Int J Cancer Suppl 12: 58-64, 1999.
- Armstrong FD, Toledano SR, Miloslavich K, et al.: The Miami pediatric quality of life questionnaire: parent scale. Int J Cancer Suppl 12: 11-7, 1999.
- Calaminus G, Weinspach S, Teske C, et al.: Quality of life in children and adolescents with cancer. First results of an evaluation of 49 patients with the PEDQOL questionnaire. Klin Padiatr 212 (4): 211-5, 2000 Jul-Aug.
- Vannatta K, Gartstein MA, Short A, et al.: A controlled study of peer relationships of children surviving brain tumors: teacher, peer, and self ratings. J Pediatr Psychol 23 (5): 279-87, 1998.
- Phipps S, Mulhern RK: Family cohesion and expressiveness promote resilience to the stress of pediatric bone marrow transplant: a preliminary report. J Dev Behav Pediatr 16 (4): 257-63, 1995.
- Casillas JN, Zebrack BJ, Zeltzer LK: Health-related quality of life for Latino survivors of childhood cancer. J Psychosoc Oncol 24 (3): 125-45, 2006.
- Barrera M, Wayland LA, D'Agostino NM, et al.: Developmental differences in psychological adjustment and health-related quality of life in pediatric cancer patients. Child Health Care 32 (3): 215-32, 2003.
- Phipps S, Fairclough D, Mulhern RK: Avoidant coping in children with cancer. J Pediatr Psychol 20 (2): 217-32, 1995.
- Sorgen KE, Manne SL: Coping in children with cancer: examining the goodness-of-fit hypothesis. Child Health Care 31 (3): 191-207, 2002.
- Hamama R, Ronen T, Feigin R: Self-control, anxiety, and loneliness in siblings of children with cancer. Soc Work Health Care 31 (1): 63-83, 2000.
- Alderfer MA, Labay LE, Kazak AE: Brief report: does posttraumatic stress apply to siblings of childhood cancer survivors? J Pediatr Psychol 28 (4): 281-6, 2003.
- Sargent JR, Sahler OJ, Roghmann KJ, et al.: Sibling adaptation to childhood cancer collaborative study: siblings' perceptions of the cancer experience. J Pediatr Psychol 20 (2): 151-64, 1995.
- MacLeod KD, Whitsett SF, Mash EJ, et al.: Pediatric sibling donors of successful and unsuccessful hematopoietic stem cell transplants (HSCT): a qualitative study of their psychosocial experience. J Pediatr Psychol 28 (4): 223-30, 2003.
- Packman W: Psychosocial impact of pediatric BMT on siblings. Bone Marrow Transplant 24 (7): 701-6, 1999.
- Houtzager BA, Grootenhuis MA, Last BF: Supportive groups for siblings of pediatric oncology patients: impact on anxiety. Psychooncology 10 (4): 315-24, 2001 Jul-Aug.
- Murray JS: Self-concept of siblings of children with cancer. Issues Compr Pediatr Nurs 24 (2): 85-94, 2001 Apr-Jun.
- Zebrack BJ, Zevon MA, Turk N, et al.: Psychological distress in long-term survivors of solid tumors diagnosed in childhood: a report from the childhood cancer survivor study. Pediatr Blood Cancer 49 (1): 47-51, 2007.
- Zeltzer LK, Lu Q, Leisenring W, et al.: Psychosocial outcomes and health-related quality of life in adult childhood cancer survivors: a report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev 17 (2): 435-46, 2008.
- Lown EA, Goldsby R, Mertens AC, et al.: Alcohol consumption patterns and risk factors among childhood cancer survivors compared to siblings and general population peers. Addiction 103 (7): 1139-48, 2008.
- Ness KK, Gurney JG, Zeltzer LK, et al.: The impact of limitations in physical, executive, and emotional function on health-related quality of life among adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Arch Phys Med Rehabil 89 (1): 128-36, 2008.
- Mulrooney DA, Ness KK, Neglia JP, et al.: Fatigue and sleep disturbance in adult survivors of childhood cancer: a report from the childhood cancer survivor study (CCSS). Sleep 31 (2): 271-81, 2008.
Latest Updates to This Summary (04 / 12 / 2023)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
Overview
Updated National Comprehensive Cancer Network (NCCN) as reference 5.
Definitions
Updated NCCN as reference 4.
Screening and Assessment
Updated NCCN as reference 9.
Normal Adjustment
Added text about a prospective observational study of 243 adult cancer survivors who were referred for psycho-oncology services. The study found that participants' depression and distress scores were significantly lower at the second visit than at baseline, and that the differences in scores were clinically meaningful and did not differ by clinician type (cited Molinaro et al. as reference 38 and level of evidence II).
Psychosocial Distress
Updated NCCN as reference 1.
Anxiety Disorders: Description and Etiology
Revised text to state that severe pain or other physical symptoms can increase the likelihood of developing anxiety disorders during cancer treatment (cited Suskin et al. as reference 8).
This summary is written and maintained by the
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about normal adjustment issues, and the pathophysiology and treatment of psychosocial distress and the adjustment disorders. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Adjustment to Cancer are:
- Natalie Jacobowski, MD (Nationwide Children's Hospital)
- Jayesh Kamath, MD, PhD (University of Connecticut Health Center)
- Tammy I. Kang, MD, MSCE, FAAHPM (Texas Children's Pavilion for Women)
- Maryam B. Lustberg, MD, MPH (Yale University School of Medicine)
- Edward B. Perry, MD (VA Connecticut Healthcare System)
- Rachel A. Pozzar, PhD, RN (Dana-Farber Cancer Institute)
- Amy Wachholtz, PhD, MDiv, MS, ABPP (University of Colorado)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Supportive and Palliative Care Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary]."
The preferred citation for this PDQ summary is:
PDQ® Supportive and Palliative Care Editorial Board. PDQ Adjustment to Cancer. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at:
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in
Disclaimer
The information in these summaries should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our
Last Revised: 2023-04-12
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the
Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.
Page Footer
I want to...
Audiences
Secure Member Sites
The Cigna Group Information
Disclaimer
Individual and family medical and dental insurance plans are insured by Cigna Health and Life Insurance Company (CHLIC), Cigna HealthCare of Arizona, Inc., Cigna HealthCare of Illinois, Inc., Cigna HealthCare of Georgia, Inc., Cigna HealthCare of North Carolina, Inc., Cigna HealthCare of South Carolina, Inc., and Cigna HealthCare of Texas, Inc. Group health insurance and health benefit plans are insured or administered by CHLIC, Connecticut General Life Insurance Company (CGLIC), or their affiliates (see
All insurance policies and group benefit plans contain exclusions and limitations. For availability, costs and complete details of coverage, contact a licensed agent or Cigna sales representative. This website is not intended for residents of New Mexico.