Liver Cancer Causes, Risk Factors, and Prevention
Worldwide, liver cancer is the sixth most common cancer and the third leading cause of cancer death. In the United States, rates are highest in American Indian or Alaska Native individuals. Liver cancer is the sixth leading cause of cancer deaths in the United States.
Liver cancer causes and risk factors
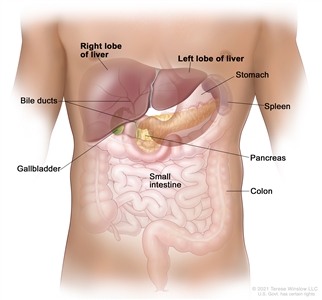
The most common type of liver cancer in adults, hepatocellular carcinoma (HCC), typically develops in people with chronic (long-lasting) liver disease caused by hepatitis virus infection or cirrhosis. Men are more likely to develop HCC than women. People with multiple risk factors have an even higher risk.
Many risk factors have been associated with liver cancer. Not everyone with one or more of these risk factors will develop the disease, and the disease will develop in some people who don't have any known risk factors. Risk factors include the following:
- Hepatitis B virus (HBV) infection: HBV can be transmitted in blood, semen, or other body fluids. The infection can be passed from mother to child during childbirth, through sexual contact, or by sharing needles that are used to inject drugs. It can cause inflammation (swelling) of the liver that leads to cancer. Routine HBV vaccination in infancy is reducing the incidence of HBV infection. Chronic HBV infection is the leading cause of liver cancer in Asia and Africa.
- Hepatitis C virus (HCV) infection: HCV can be transmitted in the blood. The infection can be spread by sharing needles that are used to inject drugs or, less often, through sexual contact. In the past, it was also spread during blood transfusions or organ transplants. Today, blood banks test all donated blood for HCV, which greatly lowers the risk of getting the virus from blood transfusions. It can cause cirrhosis that may lead to liver cancer. Chronic HCV infection is the leading cause of liver cancer in North America, Europe, and Japan.
- Cirrhosis: The risk of developing liver cancer is increased for people who have cirrhosis, a disease in which healthy liver tissue is replaced by scar tissue. The scar tissue blocks the flow of blood through the liver and keeps it from working as it should. Chronic alcoholism and chronic hepatitis infections are common causes of cirrhosis. People with HCV-related cirrhosis have a higher risk of developing liver cancer than people with cirrhosis related to HBV or alcohol use.
- Heavy alcohol use: Heavy alcohol use can cause cirrhosis, which is a risk factor for liver cancer. Liver cancer can also occur in heavy alcohol users who do not have cirrhosis. Heavy alcohol users who have cirrhosis are ten times more likely to develop liver cancer, compared with heavy alcohol users who do not have cirrhosis.
Studies have shown there is also an increased risk of liver cancer in people with HBV or HCV infection who use alcohol heavily.
- Aflatoxin B1: The risk of developing liver cancer may be increased by eating foods that contain aflatoxin B1 (poison from a fungus that can grow on foods, such as corn and nuts, that have been stored in hot, humid places). It is most common in sub-Saharan Africa, Southeast Asia, and China.
- Nonalcoholic steatohepatitis (NASH): NASH is a condition that can cause cirrhosis that may lead to liver cancer. It is the most severe form of nonalcoholic fatty liver disease, where there is an abnormal amount of fat in the liver. In some people, this can cause inflammation and injury to the cells of the liver.
Having NASH-related cirrhosis increases the risk of developing liver cancer. Liver cancer has also been found in people with NASH who do not have cirrhosis.
- Cigarette smoking: Cigarette smoking has been linked to a higher risk of liver cancer. The risk increases with the number of cigarettes smoked per day and the number of years the person has smoked.
- Other conditions: Certain rare medical and genetic conditions may increase the risk of liver cancer. These conditions include the following:
- untreated hereditary hemochromatosis
- alpha-1 antitrypsin deficiency
- glycogen storage disease
- porphyria cutanea tarda
- Wilson disease
Liver cancer prevention
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will lower the number of deaths caused by cancer.
Anything that increases your chance of getting cancer is called a risk factor. Anything that lowers your chance of getting cancer is called a cancer protective factor. Prevention includes avoiding risk factors and increasing protective factors.
The following are protective factors for liver cancer:
- Getting the hepatitis B vaccine: Preventing HBV infection (by being vaccinated for HBV as a newborn) has been shown to lower the risk of liver cancer in children. It is not yet known if being vaccinated lowers the risk of liver cancer in adults.
- Getting treatment for chronic hepatitis B infection: Treatment options for people with chronic HBV infection include interferon and nucleos(t)ide analog therapy. These treatments may reduce the risk of developing liver cancer.
- Reducing exposure to aflatoxin B1: Replacing foods that contain high amounts of aflatoxin B1 with foods that contain a much lower level of the poison can reduce the risk of liver cancer.
Last Revised: 2024-05-15
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.